
Advances in Leukemia Research
NCI-funded researchers are working to advance our understanding of how to treat leukemia. With advances in both targeted therapies and immunotherapies, leukemia treatment has the potential to become more effective and less toxic.
This page highlights some of the latest research in leukemia, including clinical advances that may soon translate into improved care and research findings from recent studies.
Leukemia Treatment for Adults
The mainstays of leukemia treatment for adults have been chemotherapy, radiation therapy, and stem cell transplantation. Over the last two decades, targeted therapies have also become part of the standard of care for some types of leukemia. Different types of leukemia require different combinations of therapies.
Although much progress has been made against some types of leukemia, others still have relatively poor rates of survival. And, as the population ages, there is a greater need for treatment regimens that are less toxic.
Acute Lymphoblastic Leukemia (ALL)
Combining less-toxic therapies. The intensive chemotherapy treatments used for ALL have serious side effects that many older patients cannot tolerate. Targeted therapies may have fewer side effects than chemotherapy. Researchers are developing clinical trials that will test whether combinations of these types of therapies can be used instead of chemotherapy for older patients with a form of ALL called B-cell ALL.
Using CAR T-cell therapy. CAR T-cell therapy is a type of treatment in which a patient’s own immune cells are genetically modified to treat their cancer. Currently, CAR T cells are approved for the treatment of some children and young adults with ALL. They are now being explored for use in older adults with B-cell ALL. Scientists hope that it will be possible to use CAR T-cell therapy to delay—or even replace—stem-cell transplantation in older, frailer patients.
A major challenge in treating another type of ALL, called T-cell ALL, has been that it can be resistant to chemotherapy and radiation therapy. Researchers are working to develop clinical trials to test new drugs that could potentially help counter this resistance.
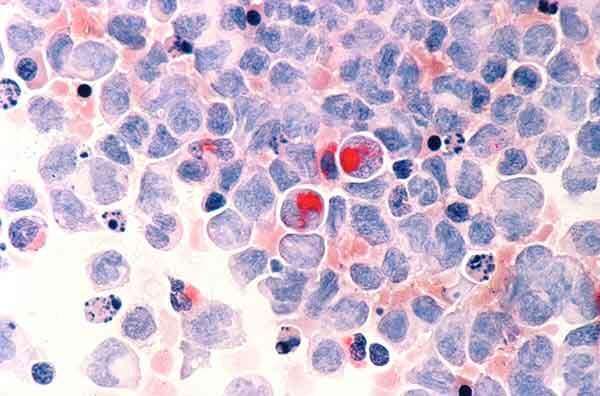
Acute Myeloid Leukemia (AML)
Targeted therapy. AML tends to be aggressive and is harder to treat than ALL. However, AML cells may have gene changes that can be targeted with new drugs. Targeted therapies that have recently been approved for AML include:
- Enasidenib (Idhifa), which inhibits the activity of mutant forms of a protein called IDH2
- Venetoclax (Venclexta), which inhibits the activity of a protein called BCL-2
- Gemtuzumab ozogamicin (Mylotarg), which targets a protein on leukemia cells called CD33 and delivers a toxin to the cells
- Midostaurin (Rydapt), which inhibits the activity of a protein called FLT3
- Gilteritinib (Xospata), which inhibits the activity of mutant forms of FLT3
- Looking at newer targeted therapies. One promising drug, called pevonedistat, targets a protein called NAE that is involved in cell division and is being studied in clinical trials.
- Studying ways to target AML cells indirectly. An ongoing clinical trial is adding the drug uproleselan to chemotherapy. Uproleselan targets a protein called E-selectin on non-cancerous cells that helps protect cancer cells from being killed by chemotherapy.
- Exploring other drugs that may have use in AML. These include HDAC inhibitors and related treatments that alter how genes are switched on and off. Many of these drugs are also being studied for the treatment of myelodysplastic syndromes (MDS), which can eventually progress to AML.
Monitoring response to treatment. The NCI-sponsored American College of Radiology Imaging Network (ACRIN) is currently running a trial to see whether positron emission tomography (PET) scanning can be used instead of bone-marrow biopsy to monitor response to treatment in people newly diagnosed with AML. If it can, PET scans would be a less invasive option for patients. PET may also be able to detect whether treatment is working earlier than is possible with biopsy, which would allow for an earlier change in therapy if required.
Chronic Myelogenous Leukemia (CML)
Most people with CML have a specific chromosome alteration called the Philadelphia chromosome, which results in the production of an abnormal protein that drives the growth of leukemia cells. Drugs that target this abnormal protein—imatinib (Gleevec), nilotinib (Tasigna), dasatinib (Sprycel), and ponatinib (Iclusig)—have radically changed the outlook for people with CML, who now have close to a normal life expectancy.
Can patients stop taking therapy? Researchers are now testing whether these drugs, which are currently taken for life, can be safely stopped in some CML patients. A clinical trial showed that some patients taking nilotinib whose cancer has been in remission for an extended period can safely stop taking the drug. These patients must still undergo regular testing to ensure the disease has not come back.
Chronic Lymphocytic Leukemia (CLL)
Refining treatment length. Recent clinical trials have shown that a combination of the drug ibrutinib (Imbruvica) with another targeted therapy benefits both younger and older patients with CLL.
In these clinical trials, patients received ibrutinib until leukemia began to grow again. Researchers would now like to test whether giving ibrutinib for a fixed amount of time and then stopping it would be as effective. This approach could potentially avoid some of the side effects of long-term treatment as well as reduce the cost of treatment.
Using CAR T-cell therapy. CAR T-cell therapy is also being tested in adults with CLL. Researchers would like to know if using this type of immunotherapy early in the course of treatment would be more effective than waiting until the cancer recurs.
Hairy Cell Leukemia (HCL)
In 2018, the Food and Drug Administration (FDA) approved moxetumomab pasudotox (Lumoxiti) for the treatment of HCL that has come back or progressed after earlier treatment. Originally discovered at NCI, the targeted therapy is the first non-chemotherapy drug approved for the disease.
Leukemia Treatment for Children
Standard leukemia treatments for children have been chemotherapy, radiation therapy, and stem-cell transplant. Despite great improvements in survival for children with some types of leukemia, some children do not respond to standard treatments or experience a relapse of their disease. Others live with the side effects of chemotherapy and radiation therapy for the rest of their lives, highlighting the need for less toxic treatments.
Now researchers are focusing on targeted drugs and immunotherapies for the treatment of leukemia in children. Newer chemotherapy drugs are also being tested.
Targeted Therapies
- About 10% of children with AML have changes in a gene called FLT3. A clinical trial is testing a drug that targets FLT3, sorafenib (Nexavar), in addition to standard chemotherapy in these children. Other trials testing drugs that target FLT3 more specifically than sorafenib are being planned.
- Some pediatric leukemias have gene fusions that drive cancer cell growth. One type of gene fusion can be targeted with a drug called larotrectinib (Vitrakvi). This drug is approved for the treatment of children with solid tumors that have this specific gene fusion. A clinical trial under development will test the drug in children with leukemia that harbors this gene fusion.
- Some children with ALL have gene fusions that may be sensitive to treatment with the targeted drug dasatinib (Sprycel). A trial conducted by the NCI-sponsored Children’s Oncology Group (COG) is currently testing dasatinib for these children.
More possible targets for the treatment of childhood cancers are discovered every year, and many new drugs that could potentially be used to treat cancers that have these targets are being tested through the Pediatric Preclinical Testing Consortium.
Immunotherapy
CAR T-cell therapy has recently generated great excitement for the treatment of children with relapsed ALL. One CAR T-cell therapy, tisagenlecleucel (Kymriah), was approved in 2017 for some children with relapsed ALL.
Many challenges remain about the use of CAR T-cell therapy in children with leukemia that researchers are now trying to address:
- Sometimes, leukemia can become resistant to tisagenlecleucel. Researchers in NCI’s Pediatric Oncology Branch have developed CAR T cells that target leukemia cells in a different way. An ongoing clinical trial is testing whether the combination of these two types of CAR T cells can provide longer-lasting remissions.
- CAR T cells are currently only approved for use in leukemia that has relapsed or proved resistant to standard treatment. A clinical trial from COG is being planned to test tisagenlecleucel as part of first-line therapy in children with ALL at high risk of relapse.
- More research is also needed to understand which children who receive CAR T cells are at high risk of developing resistance to treatment and whether strategies such as combining CAR T-cell therapy with other immunotherapies may help prevent resistance from developing.
- Some children with leukemia don’t have T cells that are healthy enough to be collected to create CAR T cells. Research is ongoing to create an “off-the-shelf” CAR T-cell therapy that doesn’t require the collection of T cells from patients.
- Other research, both in NCI’s Pediatric Oncology Branch and at other institutions, is focused on creating CAR T-cell therapies that work in other types of childhood leukemia, such as AML.
Two additional drugs that harness the body’s immune system to fight cancer have shown promise for children with leukemia:
- A drug called blinatumomab (Blincyto), attaches to both T cells and cancer cells. By bringing these cells close together, the drug helps the T cells kill the cancer cells. Blinatumomab has been approved by the FDA for children with ALL who have relapsed after initial treatment. A clinical trial conducted by COG will test whether adding blinatumomab to standard chemotherapy can reduce the risk of relapse in children with newly diagnosed ALL.
- A drug called inotuzumab ozogamicin (Besponsa), is being tested in children with relapsed B-cell ALL. This drug consists of an antibody that can bind to cancer cells linked to a drug that can kill those cells.
Chemotherapy
In addition to targeted therapies and immunotherapies, researchers are also working to develop new chemotherapy drugs for leukemia and find better ways to use existing drugs. In 2018, a large clinical trial showed that adding the drug nelarabine (Arranon) to standard chemotherapy improves survival for children and young adults newly diagnosed with T-cell ALL.
Other drugs are being tested that may make standard chemotherapy drugs more effective. These drugs include venetoclax, which has been approved for older adults with some types of leukemia and is now being tested in children.
Survivorship
Children’s developing brains and bodies can be particularly sensitive to the harmful effects of cancer treatment. Because many children treated for cancer go on to live long lives, they may be dealing with these harmful effects for decades to come.
The NCI-funded Childhood Cancer Survivor Study, ongoing since 1994, tracks the long-term harmful effects of treatments for childhood cancer and studies ways to minimize these effects. NCI also funds research into altering existing treatment regimens to make them less toxic in the long term, as well as addressing ways to help cancer survivors cope with and manage health issues stemming from cancer treatment.
NCI-Supported Research Programs
See a full list of leukemia research projects that NCI funded in FY 2017.
Many NCI-funded researchers working at the NIH campus and across the United States and the world are seeking ways to address leukemia more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer. And some is more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in leukemia.
NCI’s Leukemia Specialized Programs of Research Excellence (SPORE) promotes collaborative, interdisciplinary research. SPORE grants involve both basic and clinical/applied scientists working together. They support the efficient movement of basic scientific findings into clinical settings, as well as studies to determine the biological basis for observations made in individuals with cancer or in populations at risk for cancer.
The Pediatric Immunotherapy Discovery and Development Network (PI-DDN) is working to discover and characterize new targets for immunotherapies, design experimental models to test the effectiveness of pediatric immunotherapies, develop new immunotherapy treatments, and improve the understanding of tumor immunity in pediatric cancer patients. The PI-DDN was established as part of the Cancer Moonshot initiative.
Researchers in NCI’s Division of Cancer Epidemiology and Genetics (DCEG) are investigating novel, molecular biomarkers for leukemia, as well as clarifying relationships of established risk factors. Studies include those looking at environmental and workplace exposure, families with multiple leukemia cases, and inherited bone marrow failure syndromes to name a few.
The Fusion Oncoproteins in Childhood Cancers (FusOnC2) Consortium is also being established as part of the Cancer Moonshot initiative. The consortium of collaborating research teams will work to advance the understanding of how five important fusion oncoproteins help drive pediatric cancers, including leukemia, and apply this knowledge towards developing drugs that target these proteins.
NCI has also formed partnerships with the pharmaceutical industry, academic institutions, and individual investigators for the early clinical evaluation of innovative cancer therapies. The Experimental Therapeutics Clinical Trials Network (ETCTN) was created to evaluate these therapies using a coordinated, collaborative approach to early-phase clinical trials.
The Pediatric Early-Phase Clinical Trials Network was established to help identify and develop effective new drugs for children and adolescents with cancer. The network’s focus is on phase I and early phase II trials, as well as pilot studies of novel drugs and treatment regimens to determine their tolerability.
NCI’s Pediatric Preclinical Testing Consortium develops mouse models to allow early, rapid testing of new drugs for pediatric cancers, including leukemia. The models are all derived from tissue samples taken from patients’ tumors. The consortium partners both with commercial drug companies and with drug development efforts at universities and cancer centers.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Find leukemia-related trials from NCI's list of cancer clinical trials now accepting patients.
Leukemia Research Results
The following are some of our latest news articles on leukemia research:
- Combination Therapy with Venetoclax Approved for Chronic Lymphocytic Leukemia
- Tagraxofusp Proves Effective for BPDCN, A Rare Blood Cancer
- Treatment for Children with Leukemia Also Effective for Adolescents, Young Adults
- FDA Approvals Bring New Options for Older Patients with AML
- Drug Combination May Target the Unique Metabolism of Leukemia Stem Cells
- Ibrutinib Plus Rituximab Superior to Standard Treatment for Some Patients with Chronic Leukemia
View the full list of Leukemia Research Results and Study Updates.





























No hay comentarios:
Publicar un comentario