
Modified Stem Cells Deliver Chemotherapy to Metastatic Tumors
August 30, 2017, by NCI Staff
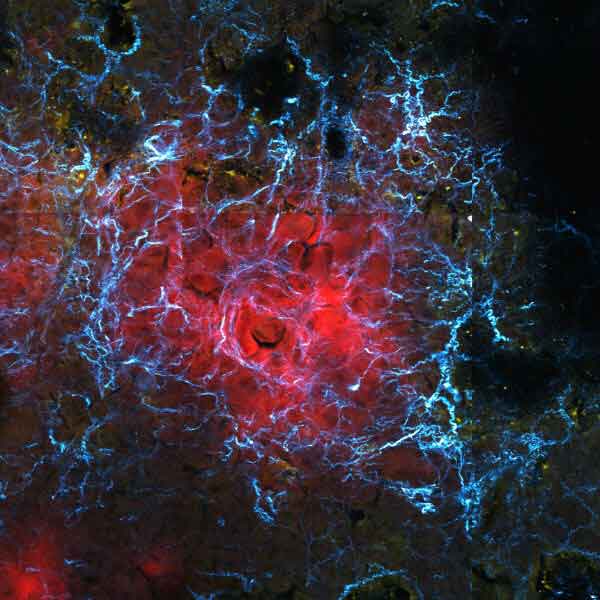
Researchers have used modified stem cells to deliver a cancer drug selectively to metastatic breast cancer tumors in mice. The stem cells specifically targeted metastatic tumors by homing in on the stiff environment that typically surrounds them.
Compared with nonmodified stem cells, the modified stem cell treatment shrank metastatic breast tumors in mice and improved their rate of survival. The study results were published July 26 in Science Translational Medicine.
Components in the area surrounding tumors, called the tumor microenvironment, can directly affect cancer progression and metastasis. Now, the research team believes, they may have found a way to take advantage of the tumor microenvironment.
In contrast to other therapies that target cancer cells directly, “we demonstrated that you can actually target the ‘home’ where cancer cells reside—the tumor microenvironment,” said the study’s lead investigator, Weian Zhao, Ph.D., of University of California, Irvine.
“The concept of the study is novel and very promising therapeutically. It is a great proof of principle. Although there remains a lot of details to work out, it has the potential to change the way we treat patients at high risk for metastasis,” said Rosandra Kaplan, M.D., head of the Tumor Microenvironment Section of NCI’s Center for Cancer Research, who was not involved in the study.
An exciting characteristic of the approach, Dr. Kaplan continued, is that it is adjustable and dynamic, which means that it may potentially be fine-tuned to an individual patient’s needs.
“When you give a patient a big whopping dose of chemotherapy, it’s like a bomb,” she said. “This is more like Navy Seal stealth action, like knowing what position to get in and exactly when to pull the trigger. There’s a lot of promise there.”
A Stiff Microenvironment
Although metastatic cancer accounts for the majority of cancer deaths, no currently available cancer treatment specifically targets metastatic tumors. Dr. Zhao and his colleagues wondered whether specific components of the tumor microenvironment might allow them to zero in on metastatic tumors.
Within the tumor microenvironment, a latticework of fibrous molecules called the extracellular matrix provides a “foundation for cells to communicate information with each other and a set of train tracks, if you will, for them to move on,” explained Dr. Kaplan. In addition, the physical stiffness of the matrix can influence the behavior of nearby cells.
For example, when breast cancer cells metastasize, they tend to settle in stiff extracellular matrices in the lungs. Signals and cues from the extracellular matrix help the cancer cells survive and grow in their new environment, she continued.
A stiff matrix in the microenvironment can also affect gene expression and development of a kind of adult stem cell, called mesenchymal stem cells (MSCs), which helps repair injured tissues. Specifically, if these stem cells—which can develop into several different cell types—encounter a more rigid matrix, they become bone cells. But if they are in in a more flexible matrix, they turn into fat cells.
In addition, MSCs preferentially settle near tumors, and some researchers think that the stiff microenvironment may help recruit them.
Because of the properties of MSCs, Dr. Zhao and his team reasoned that these cells might be used to specifically target tumors. While the researchers focused on metastatic tumors in their current study, their approach could theoretically “target primary tumors as well,” Dr. Zhao said.
To manipulate MSCs into delivering cancer therapy to tumors, the researchers modified the cells so that they would express the gene for a key enzyme only when they encounter a stiff microenvironment. The enzyme, called cytosine deaminase (CD), converts the chemical flucytosine into the chemotherapy drug fluorouracil.
Fluorouracil is commonly used to treat breast cancer. But like other chemotherapy drugs, it can damage healthy tissues and lead to toxicity when given systemically.
The team’s hope was that by modifying MSCs to express the CD enzyme only in the stiff tumor microenvironment, the chemotherapy drug would be activated specifically near tumors, preferentially killing cancer cells while sparing healthy cells.
Targeting Metastatic Tumors
In lab experiments, the researchers mixed the modified MSCs, breast cancer cells, and flucytosine on different surfaces. They found that the modified MSCs expressed CD and reduced breast cancer cell growth when placed on a stiff glass surface but not when placed on a soft gel surface.
Next, they implanted mice with human breast cancer cells, which eventually formed metastatic tumors in the mice’s lungs. They then injected these mice with the modified or nonmodified MSCs, and, the following day, injected them with flucytosine.
The modified MSCs homed to metastatic lung tumors and expressed CD, the researchers found, and the activated flucytosine reduced tumor size and improved survival of the mice. There was no effect, however, on tumor size or survival in mice treated with nonmodified MSCs and flucytosine.
In addition, they found that the modified MSCs did not damage healthy cells in the bone marrow, livers, or brains of mice. But when they injected mice with MSCs that constantly expressed CD, followed by an injection of flucytosine, the treatment damaged healthy tissue.
This is presumably because flucytosine was activated outside of the tumor, and it demonstrates that a targeted approach is critical to reducing its harmful side effects, Dr. Zhao said.
Dr. Kaplan said, “it’s clear that they have a means to deliver chemotherapy with potentially less toxicity, but it still may cause local toxicity,” meaning it damaged healthy tissue in the area near the tumor. Another concern, she added, is that not all tumors may be sensitive to the effects of fluorouracil.
In addition, how the immune system may interact with these modified MSCs remains an open question, Dr. Kaplan noted.
“We know that, in general, cell-based therapies can be fraught with immune-related issues, such as elimination of modified cells by immune cells.”
Taking Advantage of the Microenvironment
Unmodified MSCs are currently being tested in over 100 clinical trials as experimental therapies for different diseases, including cancer, and so far have proven to be safe in humans.
The stem cells are typically collected from the bone marrow, fat, or umbilical cord tissue of a patient or an unrelated donor. So unlike other cell-based therapies, MSC-based therapies don’t require a personalized treatment for each individual patient, said Dr. Zhao. Rather, an off-the-shelf treatment for hundreds of patients can be created from MSCs obtained from a single unrelated donor, he explained.
Looking forward, the research team has NCI funding to try incorporating their approach into a type of immunotherapy called CAR T-cell therapy. While CAR T-cell therapy is a promising experimental cancer treatment, it can cause severe—sometimes life-threatening—side effects by unintentionally damaging healthy tissues.
“We are working to create CAR T-cells that not only recognize the tumor but that also have to recognize the tumor microenvironment before they activate their killing mechanism,” Dr. Zhao said. “This way, we make sure they are not just effective but safe as well.”
No hay comentarios:
Publicar un comentario