
Chest CT shows COVID-19 damage to the lungs
Several new studies present peer-reviewed cases of COVID-19 in order to ensure that the disease is diagnosed as rapidly as possible, and thus help prevent an overwhelming spike in infections in any one place during the course of the current pandemic. Much interest has been shown in the possibility of using chest X-rays, and computed tomography (CT) scans to screen for and diagnose patients with this illness, whether suspected or confirmed.
SARS-CoV-2 - Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
The illness
The novel coronavirus SARS-CoV-2 was first made known to the world on December 31, 2019, when the Chinese government apprised the World Health Organization (WHO) of the spreading of respiratory illness that closely resembled viral pneumonia, with fever, cough, and shortness of breath. This illness is now called COVID-19. The virus belongs to the same family as those that caused the SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At present, the global toll is well over 162,000, with over 6,000 deaths so far. It is essential to recognize the symptoms and signs of the disease early, not just for the sake of treating people but to ensure the infection does not spread indiscriminately.
Worldwide, about 80% of infected people recover without intensive care. About 1 in 6 infected people become critically ill with respiratory difficulty, and 3.4% of cases die. Those at higher risk for death include older people and those with coexisting illnesses.
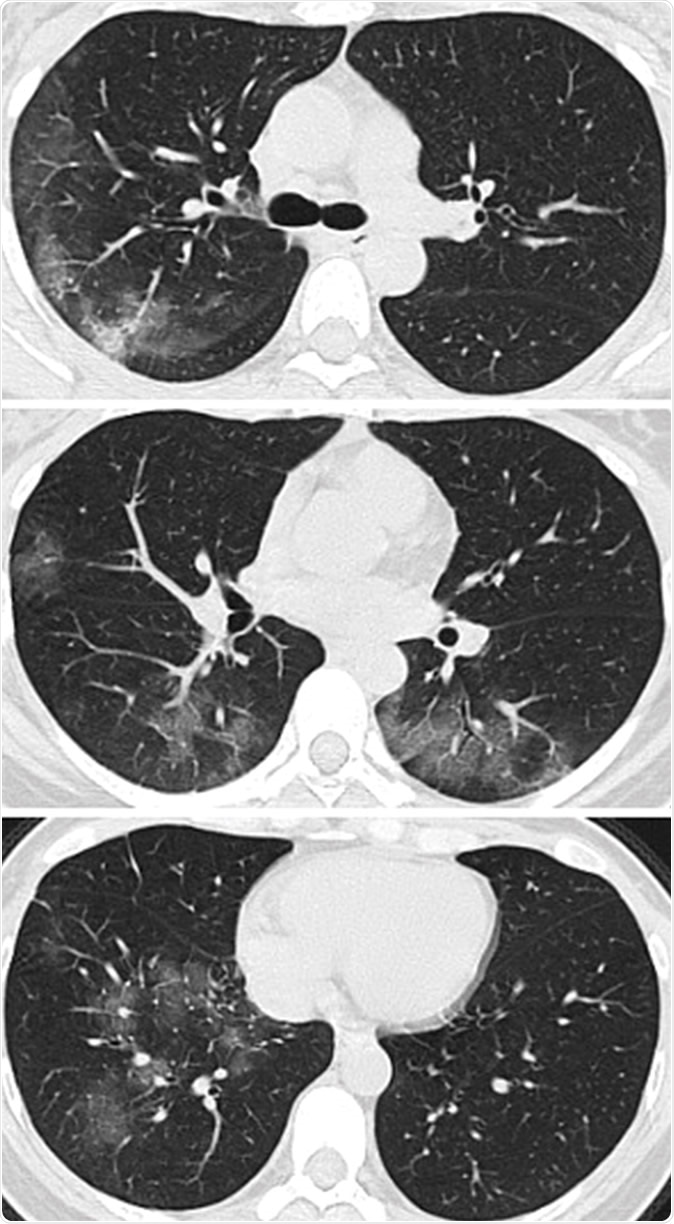
Images in a 41-year-old woman who presented with fever and positive polymerase chain reaction assay for the 2019 novel coronavirus (2019-nCoV). (a) Three representative axial thin-section chest CT images show multifocal ground glass opacities without consolidation. (b) Three-dimensional volume-rendered reconstruction shows the distribution of the ground-glass opacities (arrows). See also three-dimensional Movie (online).
The problem – and a solution?
Currently, viral testing kits are not widely available, those in use are only about 70% reliable, and many studies have shown that radiologic signs in COVID-19 patients are characteristic enough to be a useful diagnostic feature. They are very like those found in patients with SARS and MERS.
It is against this background that alternative methods of diagnosis are being explored. The medical radiology journal RSNA presents some cases of the illness to help radiologists worldwide to rapidly diagnose and thus assist in containing the spread of COVID-19.
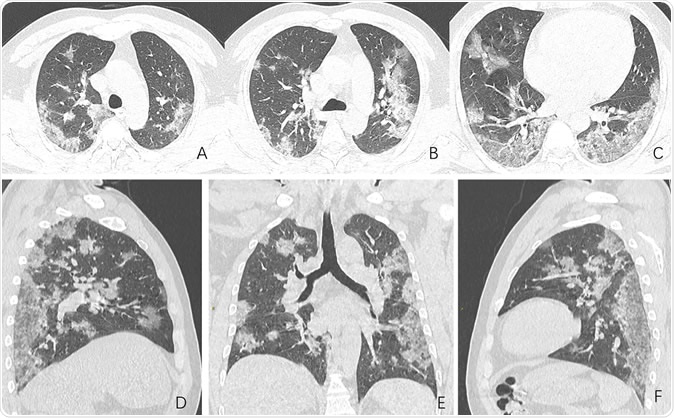
Images in a 44-year-old man who presented with fever and suspected COVID-19 pneumonia. A-C, Thin-slice (1-mm) axial CT images showed multiple patchy ground-glass opacity along the peribronchial and subpleural lungs. Some reticular opacities were also found within areas of ground glass (crazy-paving pattern). Lymphadenopathy was absent. D-F, Multiplanar reconstruction showed diffuse distribution of lesions.
The study examines the chest X-rays, and CT scans from over 20 patients aged 10-74 years, with symptoms of COVID-19. The scans showed inflamed lungs with ground-glass opacities, which look like white lung patches. These opacities are due to the partial clogging of the lung alveoli with tenacious mucus. Autopsies of Chinese patients who died of the illness because of breathing difficulties show lungs with minimal capacity for air inhalation due to the mucus accumulation.
The RSNA study shows how fluid accumulation in the lungs slowly worsens as the illness progresses, but then drains away if recovery begins until the lung spaces are completely clear.
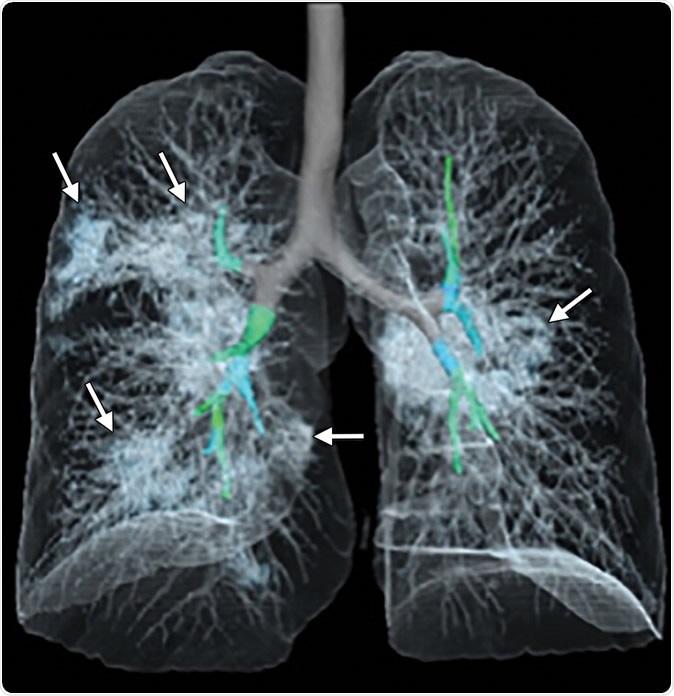
Images in a 41-year-old woman who presented with fever and positive polymerase chain reaction assay for the 2019 novel coronavirus (2019-nCoV). (a) Three representative axial thin-section chest CT images show multifocal ground glass opacities without consolidation. (b) Three-dimensional volume-rendered reconstruction shows the distribution of the ground-glass opacities (arrows). See also three-dimensional Movie (online).
The ACR position
However, despite studies showing that radiology of the chest may offer higher sensitivity for the illness, the American College of Radiology (ACR) provides the following cautions:
- Chest X-ray and CT scans are not recommended diagnostic tools at present for the diagnosis of COVID-19. The only specific method is viral testing, which should always be performed even if radiologic signs indicate the correct diagnosis.
- The first test should be viral testing of nasopharyngeal and oropharyngeal swabs, or, if available, from the lower respiratory tract.
- The ACR believes the radiologic findings are not sufficiently specific to act as a diagnostic test since similar results are present in influenza, H1N1, SARS, and MERS.
- The ACR holds that earlier trials showing the use of chest X-ray and CT scans do not improve the clinical outcome mean that these are not appropriate tests for COVID-19 diagnosis.
Current preventive measures to be taken during healthcare include:
- Asking patients suspected to have COVID-19 or the flu to avoid visiting healthcare facilities to prevent spread, as well as requiring any such visitors to wear a surgical mask and be evaluated in a closed private room.
- Radiography should be done after thorough decontamination and cleaning of any room occupied by a suspected case of COVID-19, repeated between patients, with a gap of one hour between patients unless air circulation is excellent and all the air is being replaced rapidly.
This can significantly slow down patient care, however. Given these issues, the ACR says imaging tests are to be used only as a second-line test to diagnose COVID-19, in patients with symptoms who are in hospital, have indications for CT, and with prescribed infection control procedures. Portable X-ray machines should be used if necessary, to avoid bringing infected patients into the radiology facility. Radiologists should be familiar with CT and chest X-ray appearances in COVID-19 to accelerate diagnosis even if the victim is being imaged for another indication.
The RSNA is facilitating these goals through a series of resources aimed at helping radiologists differentiate pneumonia caused by COVID-19 from viral pneumonia, including over 1000 chest CT scans.
Sources:
- Acr.org. (2020). ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
- Christian, B., (2020). Shocking X-ray images show affect of coronavirus on lungs of patients. https://www.standard.co.uk/news/world/coronavirus-symptoms-x-ray-show-affect-a4385246.html
- rsna.org. (2020). Radiologists describe coronavirus effect on the lungs. https://www.rsna.org/en/news/2020/January/Coronavirus-Update
Journal references:
- Severe Acute Respiratory Disease in a Huanan Seafood Market Worker: Images of an Early Casualty Lijuan Qian, Jie Yu, and Heshui Shi Radiology: Cardiothoracic Imaging 2020 2:1, https://pubs.rsna.org/doi/10.1148/ryct.2020200033
- 019 Novel Coronavirus (2019-nCoV) Pneumonia Peng Liu and Xian-zheng Tan, https://pubs.rsna.org/doi/10.1148/radiol.2020200257#v1
- FDG PET/CT of COVID-19 Sijuan Zou and Xiaohua Zhu, https://pubs.rsna.org/doi/10.1148/radiol.2020200770
- Essentials for Radiologists on COVID-19: An Update—Radiology Scientific Expert Panel Jeffrey P. Kanne, Brent P. Little, Jonathan H. Chung, Brett M. Elicker, and Loren H. Ketai, https://pubs.rsna.org/doi/10.1148/radiol.2020200527

































No hay comentarios:
Publicar un comentario