
About Antimicrobial Resistance
About Resistance
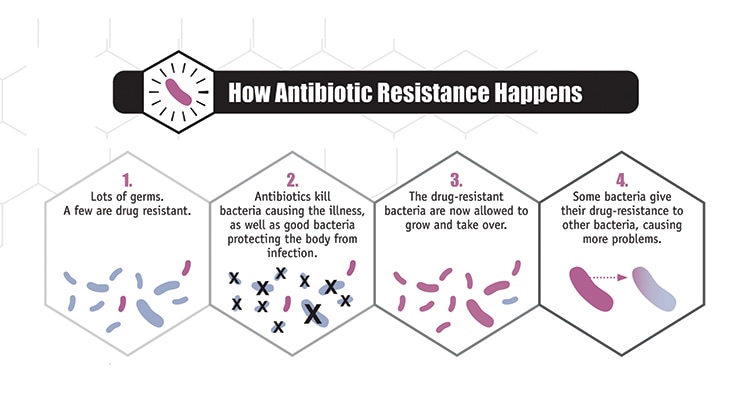
Antibiotic / Antimicrobial resistance is the ability of microbes to resist the effects of drugs – that is, the germs are not killed, and their growth is not stopped. Although some people are at greater risk than others, no one can completely avoid the risk of antibiotic-resistant infections. Infections with resistant organisms are difficult to treat, requiring costly and sometimes toxic alternatives.
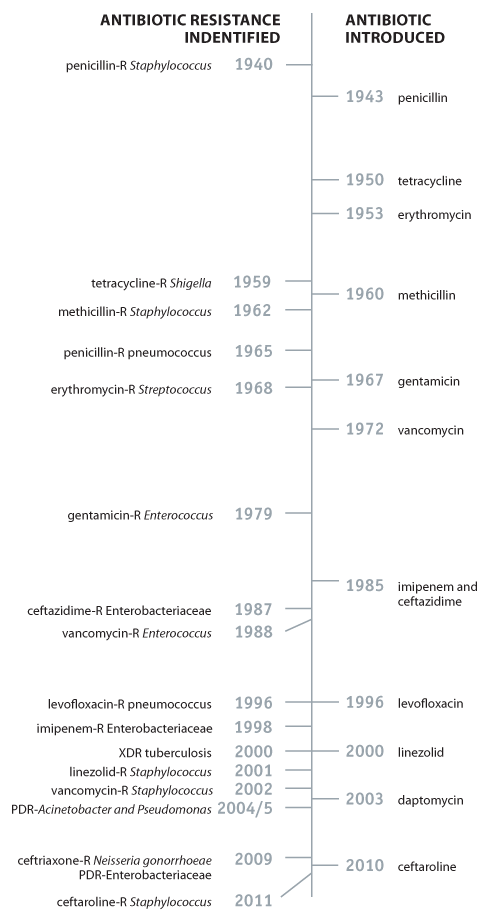
Bacteria will inevitably find ways of resisting the antibiotics developed by humans, which is why aggressive action is needed now to keep new resistance from developing and to prevent the resistance that already exists from spreading.
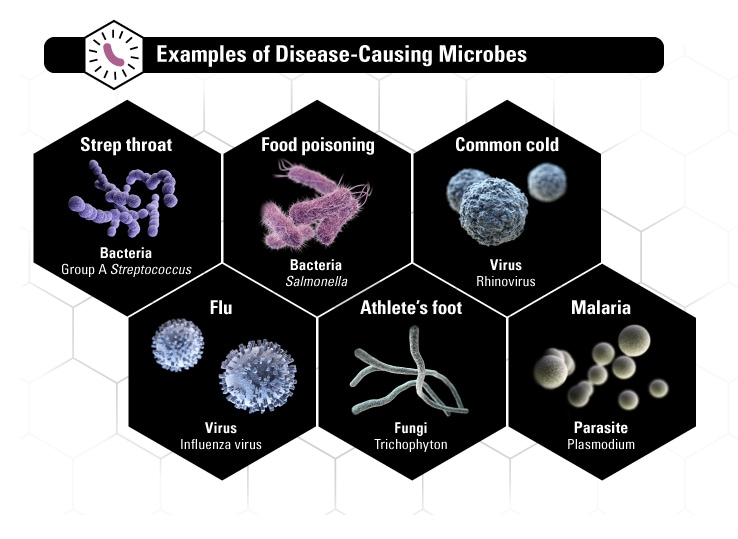
Explanation of Bacteria and Other Microbes
Microbes are organisms too small for the eye to see and are found everywhere on Earth. There are many types of microbes: bacteria, viruses, fungi, and parasites. While most microbes are harmless and even beneficial to living organisms, some can cause disease among humans, other animals, and plants. These disease-causing microbes are called pathogens; sometimes they are referred to as “germs” or “bugs.” All types of microbes have the ability to develop resistance to the drugs created to destroy them, becoming drug-resistant organisms.
How Resistance Happens
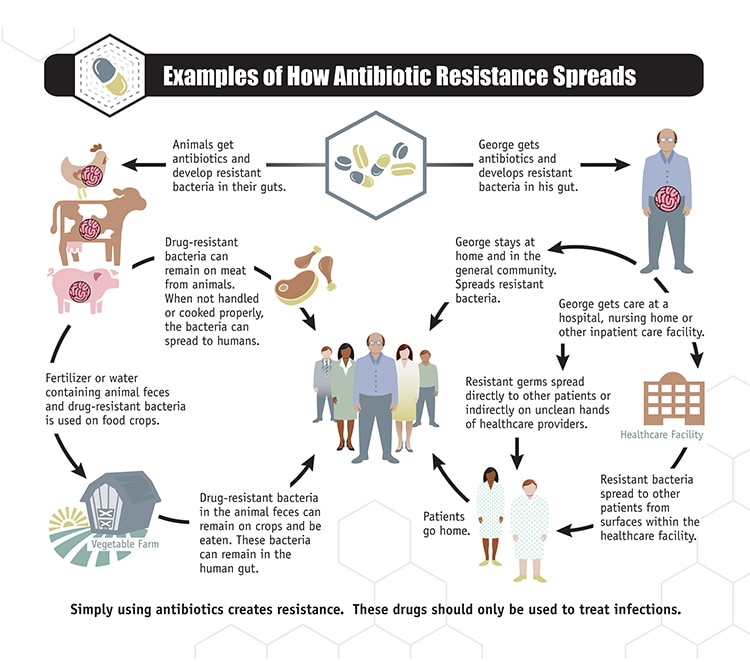
Simply using antibiotics creates resistance. These drugs should only be used to manage infections.
Trends in Drug Resistance
- Antibiotics are among the most commonly prescribed drugs used in human medicine and can be lifesaving drugs. However, up to 50% of the time antibiotics are not optimally prescribed, often done so when not needed, incorrect dosing or duration.
- The germs that contaminate food can become resistant because of the use of antibiotics in people and in food animals. For some germs, like the bacteria Salmonella and Campylobacter, it is primarily the use of antibiotics in food animals that increases resistance. Because of the link the between antibiotic use in food-producing animals and the occurrence of antibiotic-resistant infections in humans, antibiotics that are medically important to treating infections in humans should be used in food-producing animals only under veterinary oversight and only to manage and treat infectious disease, not to promote growth.
- The other major factor in the growth of antibiotic resistance is spread of the resistant strains of bacteria from person to person, or from the non-human sources in the environment.
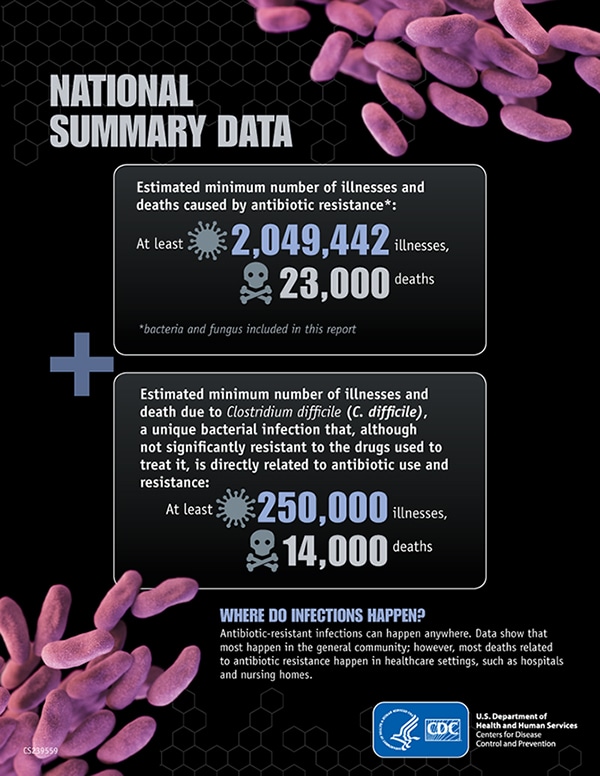
Resistance in the United States
Four Core Actions to Fight Resistance
Brief History of Antibiotics
Humans developed antimicrobials to destroy disease-causing microbes. The most commonly known antimicrobials are antibiotics, which target bacteria. Other forms of antimicrobials are antivirals, antifungals, and antiparasitics.
Penicillin, the first commercialized antibiotic, was discovered in 1928 by Alexander Fleming. While it wasn’t distributed among the general public until 1945, it was widely used in World War II for surgical and wound infections among the Allied Forces. It was hailed as a “miracle drug” and a future free of infectious diseases was considered. When Fleming won the Nobel Prize for his discovery, he warned of bacteria becoming resistant to penicillin in his acceptance speech.






















.png)









No hay comentarios:
Publicar un comentario