
Laboratory tests can help guide patient treatment, detect emerging threats, and prevent the spread of antibiotic resistance. CDC’s Antibiotic Resistance Laboratory Network (AR Lab Network) supports nationwide lab capacity to:
- rapidly detect antibiotic resistance in healthcare, food, and the community
- inform local responses to prevent spread and protect people
The AR Lab Network includes labs in 50 states, five cities, and Puerto Rico, including seven regional labs and the National Tuberculosis Molecular Surveillance Center (National TB Center).
Types of Resistance Tests
Colonization Screening
Colonization screening is a process set up to detect and reduce the risk of germs spreading in a healthcare facility (in this case, germs with unusual resistance). Some people can carry germs without becoming sick or showing symptoms, known as colonization.
People who are colonized can spread the germs to others without knowing it. When unusual resistance is identified in a patient, healthcare workers screen other patients to see if they are colonized with the same resistant germ. This can prompt additional infection control actions reducing the risk of spread and protect patients.
Identification of Pathogens
Laboratories work to identify and confirm the genus and species of pathogens (disease-causing germs) with resistance. These are often the first tests performed by the AR Lab Network. This is done through one of two methods:
- Biochemical tests: Classifying a particular species by the way it uses different biological chemicals, like proteins or sugars
- Mass spectrometry: A specialized technique that looks for a pathogen’s protein “fingerprint”
Molecular Testing
Molecular testing is a collection of techniques used to detect specific genes within a germ, including those that have and can share resistance. These tests can be used to diagnose infections and guide treatment for patients.
Phenotypic Carbapenemase Test
A phenotypic carbapenemase test uses culture (a medium to grow bacteria) instead of the molecular test method to determine if the pathogen produces an enzyme called carbapenemase. If carbapenemase is produced, then a carbapenem antibiotic is ineffective and will not kill the pathogen.
Susceptibility Testing
Susceptibility testing is a type of lab test that cultures (grows) the pathogen in order to show how sensitive a germ is to different antibiotics. These tests can be used to help select the best drug choice for a drug-resistant infection, and also provide data to monitor how a pathogen’s resistance profile might change over time.
Whole Genome Sequencing (WGS)
WGS is a laboratory procedure that provides a very precise DNA fingerprint that can help link cases to one another, allowing an outbreak to be detected and solved sooner.
How the AR Lab Network Works
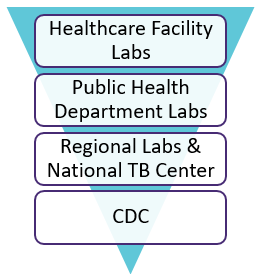
The AR Lab Network increases and sustains lab capacity nationwide. This effort between healthcare facility labs and public health department labs, regional labs and the National TB Center, and CDC results in a more rapid response for finding antibiotic resistance and preventing its spread.
Healthcare Facility Labs and Public Health Department Labs
When healthcare facility labs suspect CRE or carbapenem-resistant Pseudomonas aeruginosa (CRPA), they send the isolates (pure samples of a germ) to the public health department labs, also known as jurisdictional labs. The public health labs confirm the species identity of the bacteria, and do additional susceptibility and molecular testing to characterize (describe) the CRE and CRPA isolates. In addition to CRE and CRPA, every state health department can test for enteric (gut) bacteria like Salmonella. When public health labs identify unusual resistance, they notify CDC and can send the isolates to their regional labs for additional testing if needed.
Regional Labs and National TB Center
The regional labs help track changes in resistance and identify outbreaks. Since outbreak response varies by state, the support might also vary by state or threat discovered. In general, the regional labs provide support by:
- Doing additional tests to further characterize the threat
- Providing support to respond to the threat by performing colonization screening tests for CRE or CRPA, or an emerging fungal threat like Candida auris
- Tracking and monitoring discoveries that are found
The regional labs coordinate local efforts and are located in the following state health departments:
- Maryland
- Minnesota
- New York
- Tennessee
- Texas
- Washington
- Wisconsin
The public health department labs will send some pathogen isolates, like CRE and CRPA, to the regional labs when support is needed, but the AR Lab Network receives other pathogens in different ways. For example, the regional labs are processing N. gonorrhoeae isolates through CDC activities, including two projects: Gonococcal Isolate Surveillance Project (GISP) and Strengthening the United States Response to Resistant Gonorrhea (SURRG).
This work is a key part of monitoring antibiotic-resistant gonorrhea trends to help ensure that the recommended drug treatment for gonorrhea works. The National TB Center is coordinated from the Michigan Department of Health and Human Services, and is equipped to perform WGS for isolates of M. tuberculosis in the U.S. The National TB Center receives all available isolates from the state health departments.
CDC
CDC coordinates the AR Lab Network and provides technical expertise. When antibiotic resistance threats are reported, CDC works across the different labs to support outbreak response and create tailored solutions. CDC also adds new isolates to the Antibiotic Resistance Isolate Bank for drug and diagnostic test development
































No hay comentarios:
Publicar un comentario