
Health of Gut Microbes May Affect Survival after Stem Cell Transplant
, by NCI Staff
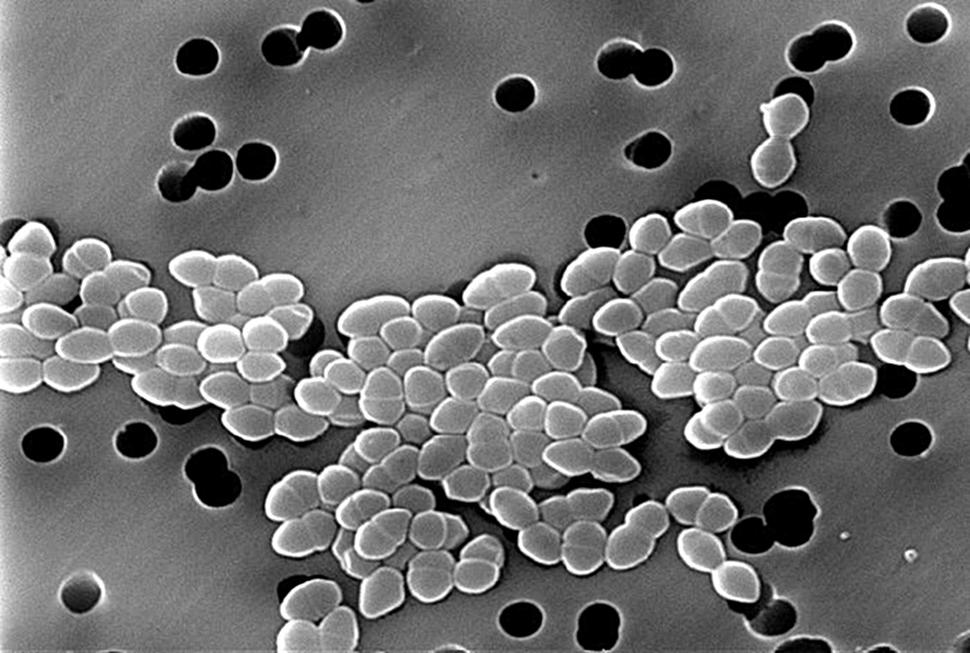
Every human body contains trillions of bacteria, viruses, and fungi that make up the normal microbiome. These microbes affect many aspects of our health. Recent studies have shown that they may play a role in cancer risk, cancer growth, and response to cancer treatments.
They also appear to affect the risk of dying after a hematopoietic stem cell transplant. In a new NCI-funded study, researchers found that, in people with blood cancers who had received an allogeneic hematopoietic stem cell transplant, the health of their gut bacteria was linked with their survival. This finding was consistent among patients treated at centers across the globe.
In an allogeneic stem cell transplant, the blood-forming stem cells in a patient’s bone marrow are destroyed using high doses of chemotherapy or radiation therapy. Stem cells from a donor, called a graft, are then infused to replace the destroyed cells, produce new marrow, and rebuild the recipient’s immune system.
This process can potentially eliminate some cancers derived from cells in the bone marrow, such as leukemia and lymphoma. It also carries risks of potential harms, including infection, graft-versus-host disease (where certain immune cells from the donor attack the normal tissue of the transplant recipient), and death.
In the new study, people whose gut microbiome became less diverse after their transplant had a higher risk of death from any cause in the weeks following treatment. (When diversity is lost, the number of different types of bacteria decrease, and in some cases the microbiome can become dominated by a single species.) People who lost diversity in their gut microbiome also had a higher likelihood of dying from graft-versus-host disease.
The study findings were published February 27 in the New England Journal of Medicine.
Although the results do not prove that the loss of microbial diversity directly influenced mortality, they highlight the importance of knowing more about how cancer treatments affect the microbiome and vice versa, explained Marcel van den Brink, M.D., Ph.D. from Memorial Sloan Kettering Cancer Center, who led the research.
More work is also needed to understand how to protect the microbiome during intensive cancer treatments such as stem cell transplantation, he added.
“One of the ways to look at the microbiome is that it’s the last organ [in the human body] that we’ve discovered,” said Dr. van den Brink. “And before you go through a stressful therapy like allogeneic transplantation, [we] want to make sure that all of your organs are functioning well.”
Questions of Consistency
Previous studies from single hospitals have shown that people undergoing allogeneic stem-cell transplantation often have disruptions in their gut microbiome, including an increase in numbers of potentially disease-causing species of bacteria and an overall loss of diversity.
These changes in the gut microbiome were associated with increased risk of harms. For example, those studies found that people whose gut bacteria became dominated by a single species had an increased risk of blood infections. And antibiotic use after transplant, which can disrupt the microbiome, is associated with a higher risk of death from any cause and specifically from graft-versus-host disease.
But it hadn’t been clear whether such risks are consistent between institutions or regions of the world.
“There are so many variables in play locally, including how we treat our patients, and environmental and genetic influences on the microbiome that vary across geographical regions,” said Steven Pavletic, M.D., a stem-cell transplant specialist at NCI’s Center for Cancer Research, who was not involved in the study.
To look more closely at whether similar changes in the gut microbiome after transplant are observed in different sites around the world, Dr. van den Brink and his colleagues looked at changes in the gut microbiome among people undergoing the procedure at four centers in three countries: two in the United States (in New York and North Carolina), one in Germany, and one in Japan.
The researchers collected almost 9,000 fecal samples from about 1,350 people undergoing allogeneic stem-cell transplantation, both before and after the procedure.
They used a type of genomic analysis called 16S ribosomal RNA sequencing to determine the types and relative abundance of bacteria in the gut at different time points. They then looked for associations between diversity of the gut microbiome and survival following transplantation, as well as the incidence of graft-versus-host disease.
Drops in Diversity
In all four centers, the team saw drops in diversity of the gut microbiome over the course of the transplantation period. The median diversity decreased by more than fourfold in New York, more than threefold in North Carolina, more than twofold in Japan, and nearly twofold in Germany.
To assess whether this loss of diversity was associated with mortality, the researchers used the median diversity found at one of the US centers as a benchmark. Across all centers, people with more than the median diversity had a lower risk of death. People with less than that median amount of diversity in the gut microbiome had about a 30% to 50% greater risk of death in the first 3 weeks after transplantation compared with those whose gut microbiome was more diverse, even after accounting for other risk factors.
The researchers also looked at the association in subgroups, including patients who received a type of transplant called a T-cell depleted graft. In this process, immune cells known as T cells are removed from the graft before transplantation. This process may reduce the risk of graft-versus-host disease.
There was no association between microbiome diversity and risk of death in people who received T-cell depleted grafts. However, among people who received grafts containing T cells, those with higher gut microbiome diversity had a lower risk of death from graft-versus-host disease specifically.
“This suggests that the loss of microbiome diversity isn’t driving the post-transplant mortality by itself,” said Dr. Pavletic. “In patients with a loss of microbiome diversity, a poor outcome following transplantation may also be driven by damage to the gastrointestinal tract, possibly caused by the T cells from the donor.
Early Disruptions
The researchers also found that, broadly, loss of diversity occurred even before patients underwent their transplant. They compared fecal samples from about 600 study participants—taken between 6 and 30 days before transplant—with about 350 samples from healthy volunteers.
The pretransplant fecal samples from people with cancer already had substantially lower bacterial diversity than those from the healthy volunteers. This early loss of diversity was associated with an increased risk of death after transplant in the New York patients but not the other groups.
Some potential explanations for this early loss include heavy use of antibiotics, damage from chemotherapy and other treatments used before transplant, and disruptions in the patients’ normal diets, explained Dr. van den Brink.
Potential Interventions and Cautions
Many potential strategies could be tested to see if supporting the microbiome can improve outcomes after stem-cell transplant, said Dr. van den Brink. These include more limited use of antibiotics, nutritional support to keep the diet balanced, and strategies to change the makeup of the microbiome directly, such as fecal transplant or use of probiotic supplements, he explained. (In a fecal transplant, fecal samples from a healthy donor a transferred to the intestines of the patient.)
Strategies to change the microbiome outright are currently risker, he added, because scientists don’t fully understand what makes up a normal, healthy microbiome.
“Everybody's trying to understand what’s a good bug, what’s a bad bug,” said Dr. van den Brink. “I think that’s too simplistic a way of trying to understand the role of the microbiome, because at the end of the day, you're dealing with an ecology. What’s living there in your gut is like a rainforest, where all these bugs work together.”
Dr. van den Brink specifically advises his patients undergoing allogeneic stem cell transplant not to try over-the-counter probiotic products on their own. Several years ago, when studies suggested that altering the microbiome may improve the efficacy of immune checkpoint inhibitors, some oncologists saw an uptick in patients taking probiotic supplements.
“But when they did a survey and looked at those patients who were doing that on their own, their outcomes were worse,” he warned. They don’t know why, but Dr. van den Brink suspects that the supplements may have negatively impacted microbial diversity.
“That's why I emphasize, don't go to the local pharmacy and start to buy the plethora of pills that are supposed to be doing something to your flora,” he said. “There's a lot that we need to learn, and there absolutely are risks.”
































No hay comentarios:
Publicar un comentario