HIV and African Americans
Blacks/African Americansa account for a higher proportion of new HIV diagnosesb and people with HIV, compared to other races/ethnicities. In 2018, blacks/African Americans accounted for 13% of the US populationc but 42% of the 37,832 new HIV diagnoses in the United States and dependent areas.d
The Numbers
HIV Diagnoses

New HIV Diagnoses Among Blacks/African Americans in the US and Dependent Areas by Transmission Category and Sex, 2018
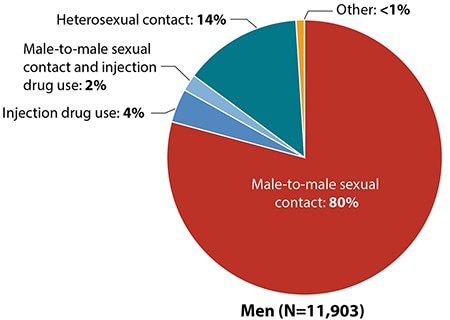
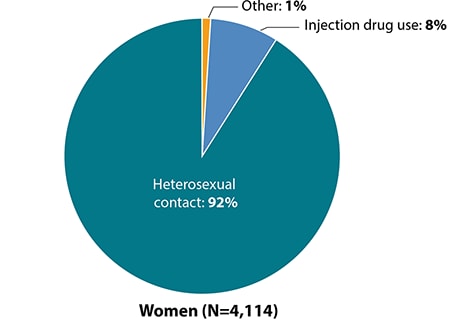
Totals may not equal 100% due to rounding.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 [PDF – 10 MB]. HIV Surveillance Report 2019;30.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 [PDF – 10 MB]. HIV Surveillance Report 2019;30.
New HIV Diagnoses in the US and Dependent Areas
for the Most-Affected Subpopulations, 2018
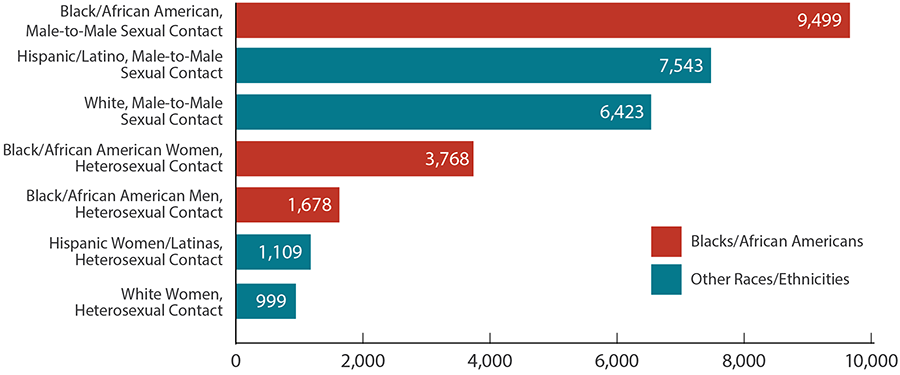
Hispanics/Latinos can be of any race.Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 [PDF – 10 MB]. HIV Surveillance Report 2019;30.
From 2010 to 2017, HIV diagnoses decreased 15% among blacks/African Americans overall in 50 states and the District of Columbia. But trends varied for different groups of blacks/African Americans.
HIV Diagnoses Among Blacks/African Americans
in the 50 States and District of Columbia, 2010-2017
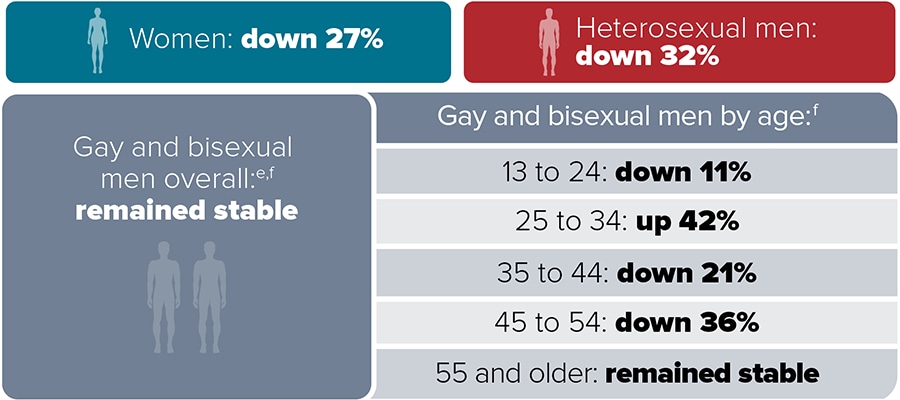
CDC. NCHHSTP AtlasPlus. Accessed January 24, 2020.
Living With HIV
Adult and Adolescent Blacks/African Americans With HIV in 50 States and the District of Columbia
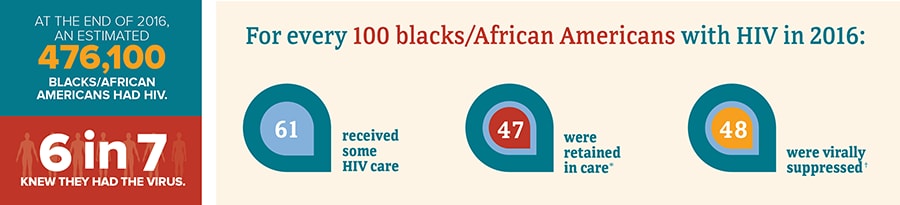

A person with HIV who takes HIV medicine as prescribed and gets and stays virally suppressed or undetectable can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners.
* Had 2 viral load or CD4 tests at least 3 months apart in a year.
† Based on most recent viral load test.
† Based on most recent viral load test.
Sources: CDC. Estimated HIV incidence and prevalence in the United States 2010–2016 [PDF – 3 MB]. HIV Surveillance Supplemental Report. 2018;24(1).
CDC. Selected national HIV prevention and care outcomes [PDF – 2 MB] (slides).
CDC. Selected national HIV prevention and care outcomes [PDF – 2 MB] (slides).
Deaths
In 2017, there were 7,053 deaths among adult and adolescent blacks/African Americans with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause.
Prevention Challenges

1 in 7 blacks/African Americans with HIV are unaware they have it. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.

African American men and women have higher rates of some sexually transmitted diseases (STDs) than other racial/ethnic communities. Having another STD can increase a person’s chance of getting or transmitting HIV.
The poverty rate among African Americans is high. The socioeconomic issues associated with poverty—including limited access to high-quality health care, housing, and HIV prevention education—directly and indirectly increase the risk for HIV infection and affect the health of people living with and at risk for HIV. These factors may explain why African Americans have worse outcomes on the HIV continuum of care, including lower rates of linkage to care and viral suppression.

Stigma, fear, discrimination, and homophobia may prevent African Americans from accessing HIV prevention and care services.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies among African Americans. Funding state, territorial, and local health departments is CDC’s largest investment in HIV prevention.
- Under the strategic partnerships and planning cooperative agreement, CDC funds the National Alliance of State and Territorial AIDS Directors to enhance health departments’ capacity to end the epidemic and supports the development and maintenance of strategic communication channels and partnerships that advance national HIV prevention goals and contribute to Ending the HIV Epidemic efforts. This award also provides funding to health departments to engage community partners in a planning process to help develop jurisdictional Ending the HIV Epidemic plans.
- In 2019, CDC awarded a cooperative agreement to strengthen the capacity and improve the performance of the nation’s HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- Under the integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2017, CDC awarded nearly $11 million per year for 5 years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and transgender youth of color, with the goal of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to key populations.
- Through its Let’s Stop HIV Together campaign, CDC provides African Americans with effective and culturally appropriate messages about HIV testing, prevention, and treatment. For example,
- Stop HIV Stigma highlights the role that each person plays in stopping HIV stigma and gives voice to people living with HIV, as well as their friends and family.
- Doing It motivates all adults to get tested for HIV and know their status.
- Start Talking. Stop HIV. focuses on gay and bisexual men and encourages open communication between sex partners and friends about HIV prevention strategies.
- HIV Treatment Works shows how people with HIV have been successful in getting care and staying on treatment.
- Partnering and Communicating Together (PACT) raises awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including African Americans.
a Black refers to people having origins in any of the black racial groups of Africa, including immigrants from the Caribbean, and South and Latin America. African American is a term often used for Americans of African descent with ancestry in North America. Individuals may self-identify as either, both, or choose another identity altogether. This fact sheet uses African American, unless referencing surveillance data.
b HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
c The US Census Bureau’s population estimates include the 50 states, the District of Columbia, and Puerto Rico.
d Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
e The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
f Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
b HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
c The US Census Bureau’s population estimates include the 50 states, the District of Columbia, and Puerto Rico.
d Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
e The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
f Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
Additional Resources
Bibliography
Fact Sheets
Other Resources
View Page In: PDF [2M]
































No hay comentarios:
Publicar un comentario