

Breast Changes and Conditions
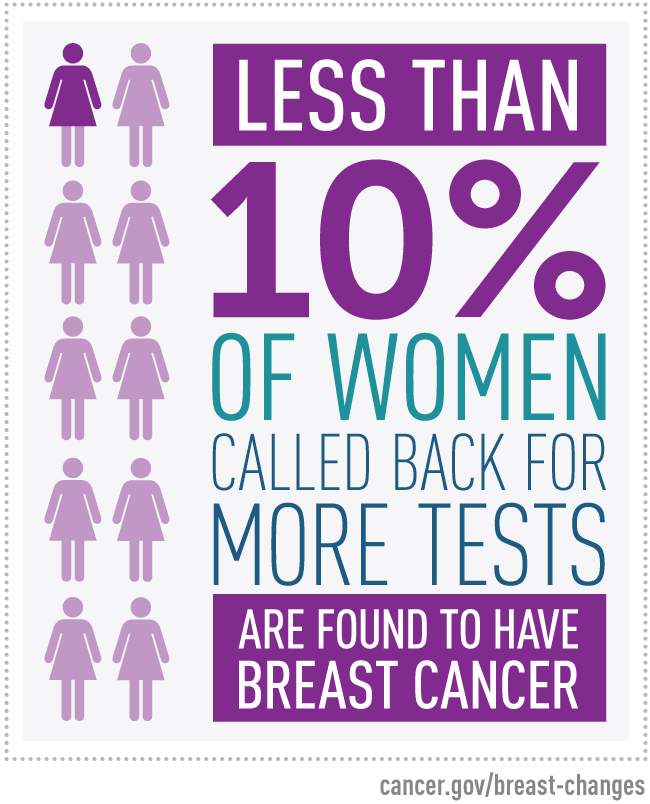
You may have just received an abnormal mammogram result, or perhaps you or your health care provider found a breast lump or other breast change. Keep in mind that breast changes are very common, and most are not cancer. This page can help you learn about symptoms during your lifetime that are not cancer as well as follow-up tests used to diagnose breast conditions and treatments for specific breast conditions.
About Breast Changes
Some breast changes can be felt by a woman or her health care provider, but most can be detected only during an imaging procedure such as a mammogram, MRI, or ultrasound. Whether a breast change was found by your doctor or you noticed a change, it’s important to follow up with your doctor to have the change checked and properly diagnosed.
Breast Changes of Concern
Check with your health care provider if your breast looks or feels different, or if you notice one of these symptoms:
- Lump or firm feeling in your breast or under your arm. Lumps come in different shapes and sizes. Normal breast tissue can sometimes feel lumpy. Doing breast self-exams can help you learn how your breasts normally feel and make it easier to notice and find any changes, but breast self-exams are not a substitute for mammograms.
- Nipple changes or discharge. Nipple discharge may be different colors or textures. It can be caused by birth control pills, some medicines, and infections. But because it can also be a sign of cancer, it should always be checked.
- Skin that is itchy, red, scaled, dimpled or puckered
Breast Changes During Your Lifetime That Are Not Cancer
Most women have changes in the breasts at different times during their lifetime.
- Before or during your menstrual periods, your breasts may feel swollen, tender, or painful. You may also feel one or more lumps during this time because of extra fluid in your breasts. Your health care provider may have you come back for a return visit at a different time in your menstrual cycle to see if the lump has changed.
- During pregnancy, your breasts may feel lumpy. This is usually because the glands that produce milk are increasing in number and getting larger. While breastfeeding, you may get a condition called mastitis. This happens when a milk duct becomes blocked. Mastitis causes the breast to look red and feel lumpy, warm, and tender. It may be caused by an infection and it is often treated with antibiotics. Sometimes the duct may need to be drained.
- As you approach menopause, your hormone levels change. This can make your breasts feel tender, even when you are not having your menstrual period. Your breasts may also feel more lumpy than they did before.
- If you are taking hormones (such as menopausal hormone therapy, birth control pills, or injections) your breasts may become more dense. This can make a mammogram harder to interpret. Be sure to let your health care provider know if you are taking hormones.
- After menopause, your hormone levels drop. You may stop having any lumps, pain, or nipple discharge that you used to have.
Diagnosing Breast Changes
Mammogram Findings
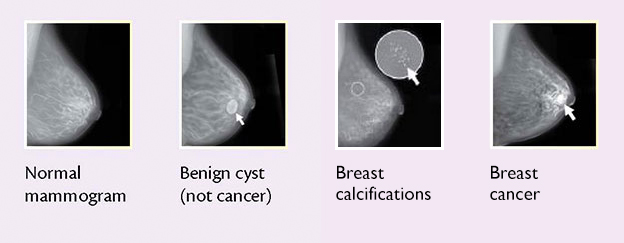
Mammograms are pictures (x-rays) of the breast, used to check for breast cancer. Possible mammogram findings include:
- Lumps (mass or tumor). Lumps come in different sizes and shapes. Fluid-filled cystsare usually smooth and rounded, with clear, defined edges and are not cancer. Lumps that have a jagged outline and an irregular shape are of more concern.
- Calcifications. There are two types of breast calcifications, or calcium deposits:
- Macrocalcifications, which look like small white dots on a mammogram. They are often caused by aging, an old injury, or inflammation and are usually benign.
- Microcalcifications, which look like white specks on a mammogram. If found in an area of rapidly dividing cells or grouped together in a certain way, they may be a sign of DCIS or breast cancer.
- Dense breast tissue: A dense breast has relatively less fat and more glandular and connective tissue. This mammogram finding is both common and normal, especially among younger women and women who use menopausal hormone therapy. Dense breast tissue can make a mammogram more difficult to interpret because both dense breast tissue and breast tumors appear as solid white areas in the image. Learn more about dense breasts and get answers to commonly asked questions.
These images are examples of breast changes that may be seen on a mammogram. You can learn more about mammograms on our Mammograms Fact Sheet.
Follow-up Tests
The procedures and tests listed below may be recommended by your health care provider to help diagnose a breast change that was found on a mammogram or that you or your health care provider felt.
Diagnostic mammography: A type of mammography in which more x-ray pictures of the breast are taken from different angles to allow a possible abnormality to be examined more closely.
Ultrasound: A procedure that makes a picture (called a sonogram) of breast tissue in order to find out if a lump is solid or is filled with fluid (that is, a cyst). Pictures are made using sound waves.
MRI (also called Magnetic Resonance Imaging): A procedure that uses a powerful magnet, radio waves, and a computer to take detailed pictures of areas inside the breast. An MRI can be used to learn more about breast lumps or large lymph nodes that were found during a clinical breast exam or breast self-exam but were not seen on a mammogram or ultrasound.
Ductography (also called a galactography): A procedure that takes pictures of the breast ducts, so that doctors can learn more about certain kinds of abnormal nipple discharge or masses such as intraductal papillomas (wart-like tumors that are benign). Pictures of the breast ducts are taken using a contrast material that is given through an injection to help breast ducts show up clearly.
Biopsy: A procedure that removes a sample of breast tissue or an entire lump so that it can be checked for signs of disease. Imaging procedures (such as ultrasound, MRIs, or x-rays) are often used during a biopsy to guide the surgeon. A pathologist then examines the sample under a microscope or performs other tests on it. Common types of breast biopsies include:
- Core needle biopsy: The use of a wide needle to remove small tissue sample(s) that are about the size of a grain of rice. It may cause a temporary bruise. Also called core biopsy.
- Fine-needle aspiration biopsy: The use of a thin needle to drain fluid and/or to remove cells.
- Surgical biopsy: The removal of part, or all, of a lump so it can be checked for signs of cancer. An incisional biopsy removes a sample of breast tissue. An excisional biopsyremoves an entire lump or suspicious area. Wire localization (also called needle localization and needle (wire) localization) may be used to mark the area of abnormal tissue before the biopsy.
- Vacuum-assisted biopsy: The removal of a small sample of breast tissue using a probe that is connected to a vacuum device. The small cut made in the breast is much smaller than with surgical biopsy. This procedure causes little scarring, and no stitches are needed. It may also be called vacuum-assisted core biopsy.
Biopsies are usually done in a doctor’s office or a clinic on an outpatient basis. This means you will go home the same day as the procedure. Local anesthesia is used for many biopsies, so you’ll be awake but won't feel pain during the procedure. General anesthesiais commonly used for surgical biopsies, which means you’ll be asleep during the procedure.
Breast Conditions and Treatment
The following alphabetical list of breast conditions includes follow-up steps and treatments that may be recommended by your health care provider. Some of these breast conditions are associated with an increased risk of breast cancer, although most are benign.
Adenosis: A benign condition of glandular tissue in the breast that may result in small round lumps, lumpiness, or lumps that are too small to be felt. If there is scar-like fibrous tissue, the condition is called sclerosing adenosis.
Atypical ductal hyperplasia (ADH): A condition in which there are more cells than normal in the breast ducts and the cells look abnormal under a microscope. Women with ADH have an increased risk of breast cancer.
- If ADH is found after a core needle biopsy, then a surgical biopsy is often recommended as the next step.
- If ADH is found and diagnosed after a surgical biopsy that takes out the entire area of ADH, follow-up care includes more frequent mammograms. Sometimes, your doctor may advise more frequent clinical breast exams and breast self-exams.
- Drugs such as tamoxifen (for all women) or raloxifene or an aromatase inhibitor (for postmenopausal women) may also be prescribed.
Atypical lobular hyperplasia (ALH): A condition in which there are more cells than normal in the breast lobules and the cells may look abnormal. Women with ALH have an increased risk of breast cancer.
- If ALH is found after a core needle biopsy, as is often the case, your doctor will talk with you about whether a surgical biopsy or more frequent mammograms are recommended.
- If ALH is found during a surgical biopsy that takes out the entire area of ALH, follow-up care generally includes only more frequent mammograms.
- Drugs such as tamoxifen (for all women) or raloxifene or an aromatase inhibitor (for postmenopausal women) may also be prescribed.
Cysts: Fluid-filled lumps that are often found in both breasts. They may be painful just before your menstrual period begins. Some cysts may be felt, while others are too small to be felt. Cysts are most common in premenopausal women and in women taking menopausal hormone therapy. Cysts are diagnosed with ultrasound and/or fine needle aspiration and usually don’t require additional treatment.
Ductal carcinoma in situ (DCIS): A condition in which abnormal cells are found in the lining of a breast duct. DCIS may also be referred to as intraductal carcinoma. In some cases, DCIS will become invasive breast cancer. Treatment is based on how much and what part of the breast is affected and how abnormal the cells look (grade). Most women with DCIS are cured with proper treatment. Treatment may include:
- Lumpectomy. This is a type of breast-conserving surgery (also called breast-sparing surgery). This may be followed by radiation therapy.
- Mastectomy. This is surgery to remove the breast or as much of the breast tissue as possible.
- Tamoxifen. This drug may also be taken to lower the chance that DCIS will come back after treatment or to prevent invasive breast cancer.
Duct ectasia (also called mammary duct ectasia): A breast condition in which the ductsin the breast thicken and become blocked with fluid, causing nipple discharge, tender or red nipples, and inverted nipples. If the blocked duct becomes infected, you may feel a lump under the nipple. Most often this condition goes away on its own and doesn’t need treatment. Your health care provider may suggest you take pain medicine; apply a warm, wet cloth to your breast; use breast pads for nipple discharge; and/or take antibiotics.
Fat necrosis: A breast condition that may cause round, firm, usually painless lumps. It may appear after an injury to the breast, surgery, or radiation therapy. Skin around the lump may look red, bruised, or dimpled. A biopsy may be used to both diagnose and remove fat necrosis.
Fibroadenoma: A benign tumor that feels like a hard, round lump in the breast. These lumps move easily and usually don't hurt. Fibroadenomas are the most common benign breast tumor in women under 30 years old. Complex fibroadenomas may slightly increase your risk of breast cancer. These lumps may go away, or your doctor may advise that they be removed.
Fibrocystic breast changes (also called fibrosis or fibrocystic breast disease): A common breast condition that causes painful, lumpy breasts. Symptoms often start before or during your menstrual period. Other changes may include sensitive nipples and itching. Fibrosis is most common among women under the age of 45 and among women taking hormone replacement therapy. As many as half of all women may have fibrocystic breast changes at some point in their lives. Although these changes are not usually treated, your health care provider may recommend that you take pain medicine, apply heat or ice compresses, and/or wear a tighter fitting bra.
Granular cell tumors: These rare tumors are almost always benign. Symptoms may include a firm lump in the breast. Surgery may be needed to remove these tumors.
Intraductal papilloma: A wart-like growth that is usually close to the nipple. It may cause pain, a lump, and clear, sticky, or bloody discharge. Single papillomas don’t increase a woman’s risk of breast cancer. However, women with multiple papillomas have an increased risk of breast cancer. A biopsy is often used to both diagnose and remove these growths.
Lobular carcinoma in situ (LCIS): A condition in which abnormal cells are found in the breast lobules. There are more abnormal cells in the lobules with LCIS than with ALH. Women with LCIS have an increased risk of developing cancer in either breast.
- If LCIS is found after a core needle biopsy, an excisional biopsy will be done.
- If LCIS is diagnosed and removed during an excisional biopsy, follow-up includes more frequent mammograms. Your doctor may also advise more frequent clinical breast exams and breast self-exams.
- Drugs such as tamoxifen (for all women) or raloxifene or an aromatase inhibitor (for postmenopausal women) may also be prescribed by your doctor.
Mastitis: A breast condition in which the breast looks red and feels lumpy, warm, and tender. It is most common among women who are breastfeeding and is caused when a milk duct becomes blocked and infected. Mastitis is commonly treated with antibiotics and can be prevented with a change in breastfeeding techniques that your doctor, nurse, or a breastfeeding consultant can help with.
Phyllodes tumor (also called CSP and cystosarcoma phyllodes): A rare type of breast tumor that is usually benign but may be cancer. In rare cases, it may spread to other parts of the body. These tumors are usually removed surgically.
Sclerosing Adenosis: A type of adenosis in which scar-like fibrous tissue is found in the glands of the breast. It may cause pain and slightly increase a woman’s risk of breast cancer. Although treatment is not usually needed, your doctor may advise taking pain medicine, making dietary changes, or wearing a bra with extra support.
































No hay comentarios:
Publicar un comentario