
A More Treatable Kind of Metastatic Cancer?
, by NCI Staff
Rarely are the terms “cure” and “metastatic cancer” used together. That’s because cancer that has spread from where it originated in the body to other organs is responsible for most deaths from the disease.
But in 1995, two cancer researchers put forth a controversial concept: There is a state of cancer metastasis that isn’t necessarily fatal. They called it oligometastatic cancer, describing it as existing between a cancer that is contained to where it originated (e.g., the breast or colon) and one that has spread extensively throughout the body.
In oligometastatic cancer, the patient has only a few, usually small metastases (“oligo” means few). For some patients, this form of metastatic cancer “should be amenable to a curative therapeutic strategy,” Ralph Weichselbaum, M.D., and Samuel Hellman, M.D., both from the University of Chicago, wrote some 25 years ago.
At the time, and still today, most people with metastatic cancer are treated only with therapies meant to kill cancer cells anywhere they may be in the body, known as systemic treatment. The assumption being that any evidence of metastatic cancer, Dr. Weichselbaum said, “means that metastases are everywhere, and that’s not necessarily true.”
That assumption, however, has also translated into the belief that direct, or “localized,” treatment of individual metastatic tumors is pointless and only subjects patients to unnecessary treatment. But that may not be the case for oligometastatic cancer, Drs. Weichselbaum and Hellman argued. Since the cancer does not appear to be widespread, perhaps treatments that directly remove the metastatic tumors, such as surgery or targeted radiation, are worthwhile.
It’s taken time, but over the last 5 years or so, the duo’s hypothesis has been put to the test, primarily in small clinical trials.
The key question is whether direct treatment of these oligometastatic tumors “can either prolong or improve the quality of life for patients?” said Bhadrasain Vikram, M.D., associate deputy director of NCI’s Radiation Research Program. “The data for that are pretty skimpy at the moment.”
The trials done to date have suggested that this approach may improve how long patients live. But Dr. Vikram and others have cited shortcomings in the studies that they say weaken their findings.
More definitive tests—in the form of larger clinical trials—are already ongoing or are in the works. What those studies find will help to shape how this concept influences patient treatment moving forward, said Joseph Salama, M.D., professor of radiation oncology at the Duke University School of Medicine.
The notion of oligometastatic cancer “is still relatively new,” Dr. Salama said. “It looks like something that could be promising for patients,” he continued, but how best to apply it “is something we’re still trying to figure out.”
Treating Everywhere… and A Few Other Places
Aggressive, systemic treatment of metastatic cancer has evolved over time. For decades, it primarily involved chemotherapy, as well as hormone treatments for cancers like breast and prostate, but now includes a growing number of targeted therapies and immunotherapy.
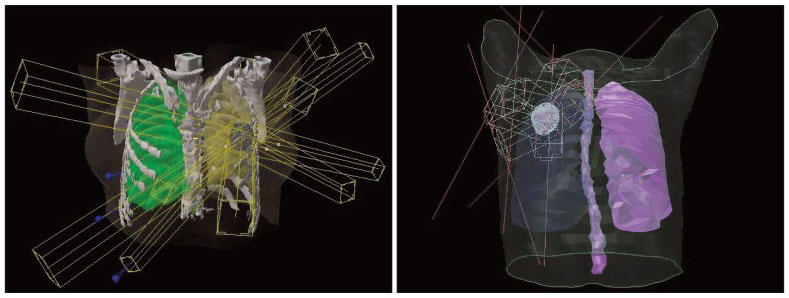
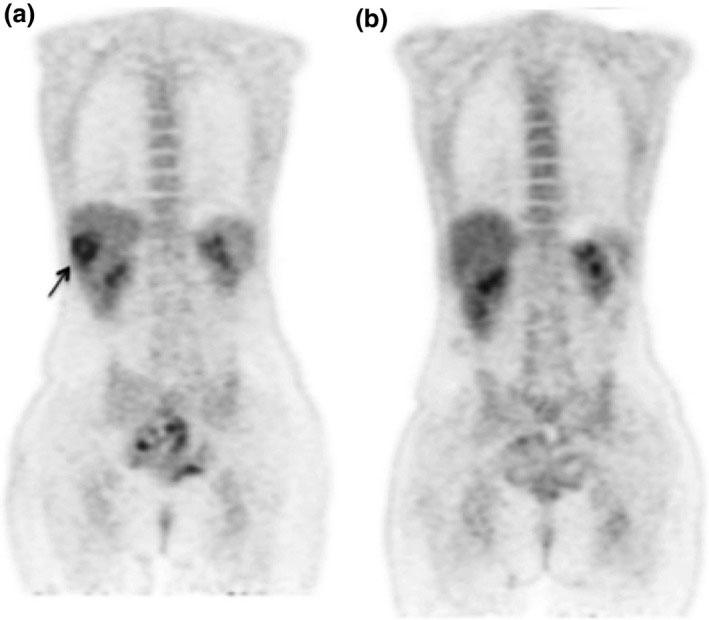
This reliance on systemic therapies is linked in part to the way in which metastatic tumors are identified—namely, imaging technologies such as PET and CT scans.
“We’re limited by the ability to accurately image metastases,” Dr. Vikram said. “Each year, [the technology] seems to get better,” he continued. But even the most cutting-edge approaches still have limitations and can’t necessarily rule out the presence of tiny deposits of tumor cells, called micrometastases, hiding in the lungs, brain, or bones.
As a consequence, treating individual metastases has not been a common part of cancer care, aside from doing so to control pain.
One situation where directly treating metastases is not uncommon is in patients with colorectal cancer that has spread to a limited number of spots on their liver. In fact, several observational studies, including one conducted in the United States and one in Europe, have reported that approximately 20% of patients initially treated with surgery to remove only their primary tumors and metastatic tumors on their liver survived for at least 10 years.
Neither study was a prospective clinical trial, however, or comprehensively documented other treatments these patients may have received.
Nevertheless, the approach is now regularly used, said Nataliya Uboha, M.D., Ph.D., of the University of Wisconsin Carbone Cancer Center, who specializes in treating gastrointestinal cancers. “We can actually cure a small percentage of patients with metastatic [colorectal cancer] that is isolated to the liver when the primary and liver tumors are completely removed surgically,” Dr. Uboha said.
She cautioned, however, that nearly all these patients would also get 3 to 6 months systemic therapy at some point during their treatment.
Putting Oligometastatic Cancer in Context
Even among cancer researchers, Dr. Weichselbaum noted, the oligometastatic concept is not always well understood. “The most important idea is that metastasis is a spectrum,” he said, both in the number of tumors and the speed at which the disease spreads.
Part of the confusion is that there’s no precise definition of oligometastatic cancer, he acknowledged.
In fact, as Dr. Salama noted, there isn’t an agreed upon number of metastases that clearly delineates oligometastatic cancer from more widespread disease. Many studies have drawn the line at five, he explained, but that number was “arbitrarily decided upon.”
But the number of metastatic tumors has to be placed in context for each patient. For example, where are the metastatic tumors located and can they safely be removed? There is also the matter of timing. Was the patient initially diagnosed with oligometastatic cancer, or was she diagnosed with a localized cancer and one or two metastases became apparent on imaging tests several months later, after a few rounds of systemic treatment?
Such distinctions are important, Dr. Uboha said, because they likely reflect the biology of the individual patient’s cancer. She cited the example of a patient initially diagnosed with widely metastatic cancer who responds well to chemotherapy and, after a period, has only one or two remaining tumors.
“Widespread disease that is down-staged with chemo, in my opinion, is still widespread disease,” she said. “Just because we don’t see it on CT scans doesn’t mean it’s completely gone.” That form of oligometastatic cancer, she believes, “represents a very different entity” than other situations in which only a few metastases have been identified.
Number Isn’t Enough
To that point, Dr. Weichselbaum said, the available data suggest that it’s not just the number of small metastatic tumors that matters. “You need to do biological characterization of the tumors,” he said.
Such information can hopefully help researchers identify specific molecular features, or “biomarkers,” that can offer insights into how aggressive a patient’s cancer is and guide the approach to treatment, he continued.
Biomarkers are desperately needed, Dr. Uboha agreed. “Right now, we look at the CT scan and we count the spots. Is that good enough? No, it’s definitely not.”
Along those lines, Drs. Weichselbaum and Hellman, in collaboration with colleagues at the University of Chicago and elsewhere, have been trying to identify molecular signatures of oligometastatic cancer.
In some of that work, they have homed in on molecules called microRNAs, whose primary function is to turn off the activity of genes. In their research, they have identified specific microRNAs that appear to influence whether metastatic tumor cells can continue their uncontrolled spread.
In one study, they identified a small group of specific microRNAs in metastatic tumor samples from people with different cancer types that was directly linked with limited spread of the disease. Further experiments in mouse models of breast cancer showed that these microRNAs blocked cancer cells’ ability to move and invade tissue, disrupting their ability to form metastases.
In more recent work, they have focused on in-depth molecular analyses of liver metastases from people with oligometastatic colorectal cancer. In that research, they discovered specific molecular features of the metastases, and those related to the immune system response, that appeared to predict how long patients survived. Such molecular patterns, the team concluded, could identify patients whose cancer is less aggressive and could thus be good candidates for direct treatment of their metastatic tumors.
While these results are promising, Dr. Weichselbaum cautioned, more research to identify and validate such biomarkers is needed before they can be used to guide everyday patient care.
Testing the Concept in Clinical Trials
The gold standard for research that typically moves the needle of cancer care is a clinical trial, particularly a large trial that randomly assigns participants to one of two (or more) groups, each of which receive different treatments.
Only a handful of randomized clinical trials have specifically enrolled patients with oligometastatic cancer and tested direct treatment of their metastatic tumors, and most of these have been relatively small.
One such trial, called SABR-COMET, enrolled approximately 100 patients with any type of solid cancer as long as they had five or fewer metastases. Participants were randomly assigned to the standard treatment for their particular cancer (control group) or the standard treatment and a targeted form of radiation called stereotactic body radiation therapy (SBRT)—also known as SABR—to treat their metastases.
When initial results were published 2 years ago, trial researchers reported that patients in the SBRT group lived more than a year longer than those in the control group.
The trial has received some criticism, however. Among the critiques is that there were many more patients with prostate cancer in the SBRT group than the control group. Prostate cancer patients with metastases live longer than patients with other metastatic cancers (e.g., lung), Dr. Vikram said, and this “imbalance” could likely have accounted for the better outcomes in that group.
In addition, three patients in the SBRT group had treatment-related deaths. Even tumor-directed treatments like SBRT “are not ‘what-do-you-have-to-lose,’” Dr. Vikram said. “It is not a risk-free enterprise.”
Other trials have only included people with specific cancers, with lung cancer being a particularly intense focus. The results thus far, albeit from small clinical trials, have been positive.
One randomized trial, for example, enrolled 29 patients with non-small cell lung cancer who had only a few metastases that after they received initial chemotherapy. Patients whose oligometastatic tumors were then treated with SBRT and additional chemotherapy lived nearly three times longer without any evidence of their cancer progressing than patients who only got additional chemotherapy. A somewhat larger trial (49 patients) had similar results.
All the trials completed to date have had notable limitations, Dr. Vikram said, such as differences in treatments that participants received. The time has come, he continued, “to move past those to larger trials, to show: Does this [approach] really make a difference?”
And that is happening. For example, a trial similar to but much larger than SABR-COMET, called SABR-COMET-3, is currently underway that is enrolling patients with any solid tumor. There is also the SABR-COMET-10 trial, which is enrolling patients with 4–10 metastases.
And Dr. Uboha is leading an NCI-funded phase 3 clinical trial enrolling people with oligometastatic esophageal and gastric cancer. To participate, patients must have no more than three metastatic tumors. They will be randomly assigned to receive either standard chemotherapy or the standard therapy along with additional radiation to all sites of their disease.
Two other NCI-supported trials of people with cancer and limited metastases include one for patients with non-small cell lung cancer and another for those with triple-negative breast cancer.
Researchers are particularly excited about the prospect of combining direct treatment of oligometastatic tumors with immunotherapy. The idea builds on a concept in cancer called the abscopal effect. Although it is thought to rarely occur in patients, the abscopal effect describes a situation where radiation delivered to a single tumor kick-starts an immune response against the cancer throughout the body.
Dr. Vikram said he is cautiously enthusiastic about studying the combination of localized radiation therapy with immunotherapy treatments like immune checkpoint inhibitors.
Rather than trying to treat “one metastatic tumor at a time, at least the ones we can see,” he said, it’s using the radiation “to help attack metastases all over the body.” As such, he continued, it may also have implications for patients with widespread metastatic cancer.
Several smaller clinical trials have tested this approach in people with NSCLC who have just a few metastases. One of those trials enrolled patients who were initially diagnosed with oligometastatic disease. In all patients, SBRT was used to treat individual metastases, which was then followed by treatment with the checkpoint inhibitor pembrolizumab (Keytruda).
Combining the two therapies did not increase the risk of serious side effects, and the results suggest that the addition of pembrolizumab may increase how long patients live without their cancer getting worse.
Dr. Salama agreed that combining local treatments like SBRT with immunotherapy looks promising. “But these [results] need to be confirmed,” he said.
There are many questions about the concept of oligometastatic cancer that still need to be answered, Dr. Salama added.
Although he believes it will eventually “help many patients” by improving their treatment, any substantial changes to everyday cancer care should wait until “we see the results of these [larger trials],” he said.
































No hay comentarios:
Publicar un comentario