
HCV and Rheumatic Disease
Hepatitis C is caused by a virus called the hepatitis C virus (HCV). It causes hepatic failure and is a frequent reason for a liver transplant.
HCV causes a host of medical conditions, including inflammation of the liver (hepatitis), the joints (arthritis), the blood vessels (vasculitis), as well as pain and weakness of the muscles. However, it is often completely asymptomatic.
Skip to
- What are the rheumatic manifestations of HCV?
- What causes rheumatic disease in HCV infection?
- What are the risk factors for HCV –related rheumatic disorders?
- Diagnosis of HCV-related rheumatic disease
- How are HCV-related rheumatic disorders treated?
- Can HCV-related joint issues be prevented?
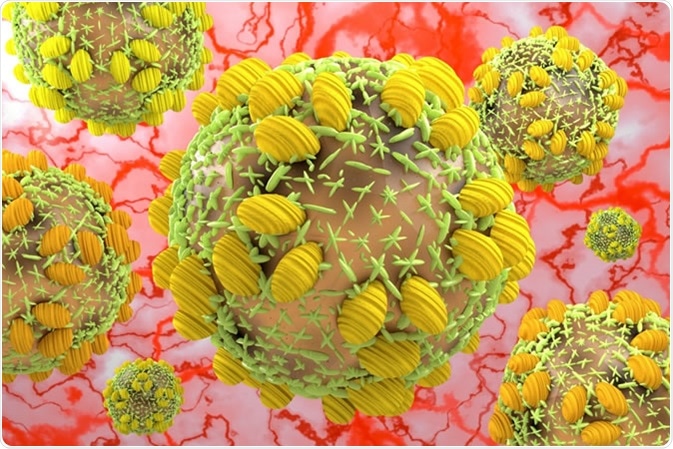
Hepatitis C virus HCV. 3D Illustration Credit: fotovapl / Shutterstock
What are the rheumatic manifestations of HCV?
HCV can cause arthritis, but also inflammation of the muscles, tendons and ligaments associated with the joints. These are called rheumatic diseases associated with HCV. Among them the most common presentation is joint pain (23%) and muscle pain (15%), with severe tiredness. Frank arthritis and vasculitis may also occur.
What causes rheumatic disease in HCV infection?
It is thought that HCV infection by itself leads to pain in the joints and muscles, but the rheumatic symptoms are also because of immune activation against the virus particles. In this case the inflammatory chemicals, or cytokines, lead to pain and swelling in other uninvolved parts of the body. Because HCV infection is often chronic, immune activation is persistent, leading to a chronically high titer of pro-inflammatory molecules in the blood. These reach joints and muscles, and constant exposure to these could cause rheumatic symptoms in the long term.
The most common HCV-related autoimmune rheumatic diseases include rheumatoid arthritis, systemic lupus erythematosus, Sjogren syndrome, polyarthritis, osteosclerosis, and antiphospholipid syndrome, among others.
What are the risk factors for HCV –related rheumatic disorders?
Both sexes and all ages are affected equally by rheumatic disease following HCV infection. No racial predilection has been observed.
Sharing needles or needlesticks with contaminated needles used for intravenous drug abuse is the most common way that HCV spreads today. Another mode of transmission is using shared utensils to snort or sniff cocaine.
Risky sexual behavior is another though somewhat less common mode of HCV spread; for this reason, people with HCV must be tested for HIV infection as well, and vice versa.
Mother-to-child transmission is also known, albeit rare.
Diagnosis of HCV-related rheumatic disease
Since HCV is asymptomatic in many cases, it is important to test for this infection when a patient with rheumatic symptoms also has risk factors for HCV.
Serological testing is employed to detect HCV infection. These are useful for screening, confirmation and for following up treatment of HCV infection.
How are HCV-related rheumatic disorders treated?
Multidisciplinary care is optimal for an HCV patient because of the wide variety of clinical features. When rheumatic disease is present, the HCV infection should be treated with the newer, non-interferon therapies, which can cure up to 97% of patients today, despite their frequent side effects.
Joint disease can be treated with new drugs that target the inflammatory molecule tumor necrosis factor- α (TNF-α), and other monoclonal antibodies used in rheumatoid arthritis.
Can HCV-related joint issues be prevented?
Since all transfused blood today is carefully screened, HCV is rarely spread in this way. All risk factors, such as sharing needles or high-risk sex, should obviously be avoided. If an individual feels he is at risk for HCV, screening is probably the best option to avoid future complications. The Centers for Disease Control and Prevention (CDC) guidelines currently advise testing for all adults born between 1945 and 1965.
Sources
- www.rheumatology.org/.../HCV-Rheumatic-Diseases
- onlinelibrary.wiley.com/.../...10)42:10%3C2204::AID-ANR24%3E3.0.CO;2-D
- https://www.nature.com/articles/nrrheum.2012.63
- https://rmdopen.bmj.com/content/1/1/e000008
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3446515/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4076875/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721975/
Further Reading
Last Updated: May 10, 2019

































No hay comentarios:
Publicar un comentario