
Causes of Abdominal Distension
Abdominal distension is a manifestation of functional gastrointestinal disorders, such as irritable bowel syndrome (IBS), and is characterized by an increase in abdominal pressure together with a visible increase in overall abdominal diameter.
Abdominal bloating, which is basically considered as a subjective sensation of abdominal heaviness, is often accompanied with abdominal distension, which is considered as an objective sign. Both bloating and distension bring discomfort and painful sensation, which altogether reduce the quality of living.
According to an epidemiological study, overall prevalence of bloating and distension in Olmsted County, Minnesota, is 19% and 9%, respectively.
According to another US study, patients with IBS and functional dyspepsia are more likely to have both bloating and distension; whereas, bloating without distension is more prevalent in patients with functional constipation.
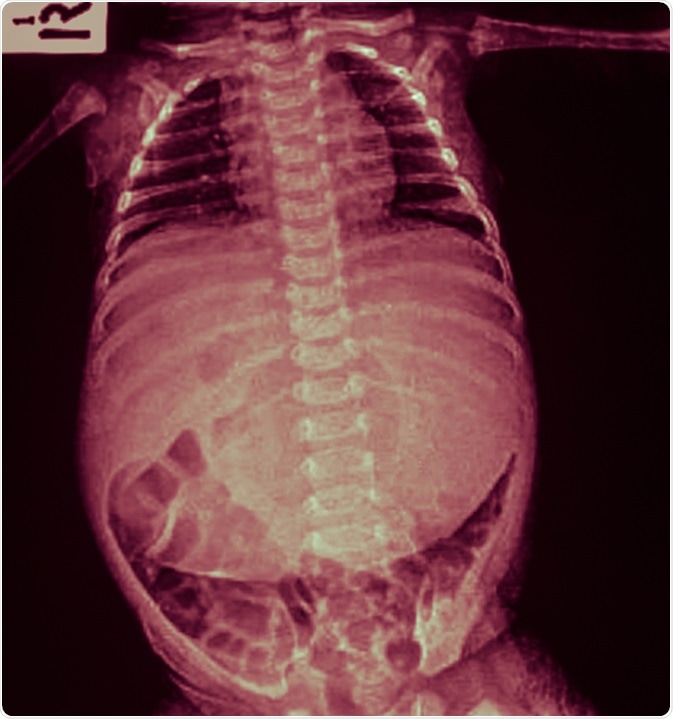
X-ray infant body and abdominal distension (flatulence, stomachache, pain). Image Credit: Tewan Banditrukkanka / Shutterstock
Contributing factors
Intestinal gas – Gas produced from the fermentation of intestinal contents is a significant contributor of abdominal distension. Poorly absorbed food components, such as lactulose, remain in the intestine after ingestion and become substrates for fermentation by gut microbiota. Moreover, an alteration in gut microbiota due to IBS or functional dyspepsia may also promote the rate of fermentation and increase intestinal gas production.
Higher water content – Poorly absorbed short-chain carbohydrates, such as fructose and mannitol, can increase the amount of water in the small-intestine by their osmotic effects. This may in turn result in abdominal distension.
Contents of the colon – Fecal impaction, which is an increase in colonic content due to constipation, can cause colon distension. In addition, increased amount of colonic content further increases the rate of fermentation and gas production. Combined effects of these incidents can significantly contribute to abdominal bloating and/or distension.
Altered intestinal gas movement – It is known that altered transit of intestinal gas, which causes undue retention of gas, is associated with episodes of abdominal distension. Probably, such alteration in gas transit is an outcome of impaired reflex control for gas clearance.
Visceral sensitivity – A change in visceral sensitivity is one of the major factors associated with abdominal distension. For example, rectal hyposensitivity, which is defined as an increased threshold for rectal distension, is a very common factor of constipation-induced abdominal distension.
Altered activity of abdominal and diaphragmatic muscle – A change in the reflex control of abdominal and diaphragmatic muscles may also cause bloating and/or distension. For instance, studies have shown that an unusual contraction of the diaphragmatic muscle and relaxation of abdominal wall muscle upon gas ingestion have been observed in patients with bloating and distension.
Altered pelvic floor function – A change in pelvic floor reflex control is also associated with abdominal distension. An altered recto-anal inhibitory reflex, a response of internal anal sphincter to rectal distension, is observed in patients with abdominal bloating, which suggests that a change in defecation process may be responsible for abdominal distension.
Pathologic aerophagia – Pathologic aerophagia occurs due to excessive swallowing of air and is also a contributing factor for abdominal distension.
Intestinal motility disorder –A reduction in gastrointestinal muscle contraction rate, such as in gastroparesis, decreases the movement of food through the gastrointestinal tract. Such condition often leads to abdominal bloating and/or distension.
Other factors – Psychological factors, such as stress and anxiety, is known to correlate with the episodes of distension. In addition, excessive bacterial growth in the small intestine may also lead to abdominal distension due to over production of gas and other fermented products.
Sources
Further Reading
Last Updated: Feb 26, 2019

































No hay comentarios:
Publicar un comentario