
Studying Genes and Proteins Together Sheds New Light on Colon Cancer
May 28, 2019, by NCI Staff
By combining the study of genes and proteins in human colon cancer tumors, scientists have discovered new features of the disease that they believe have the potential to guide novel treatment strategies.
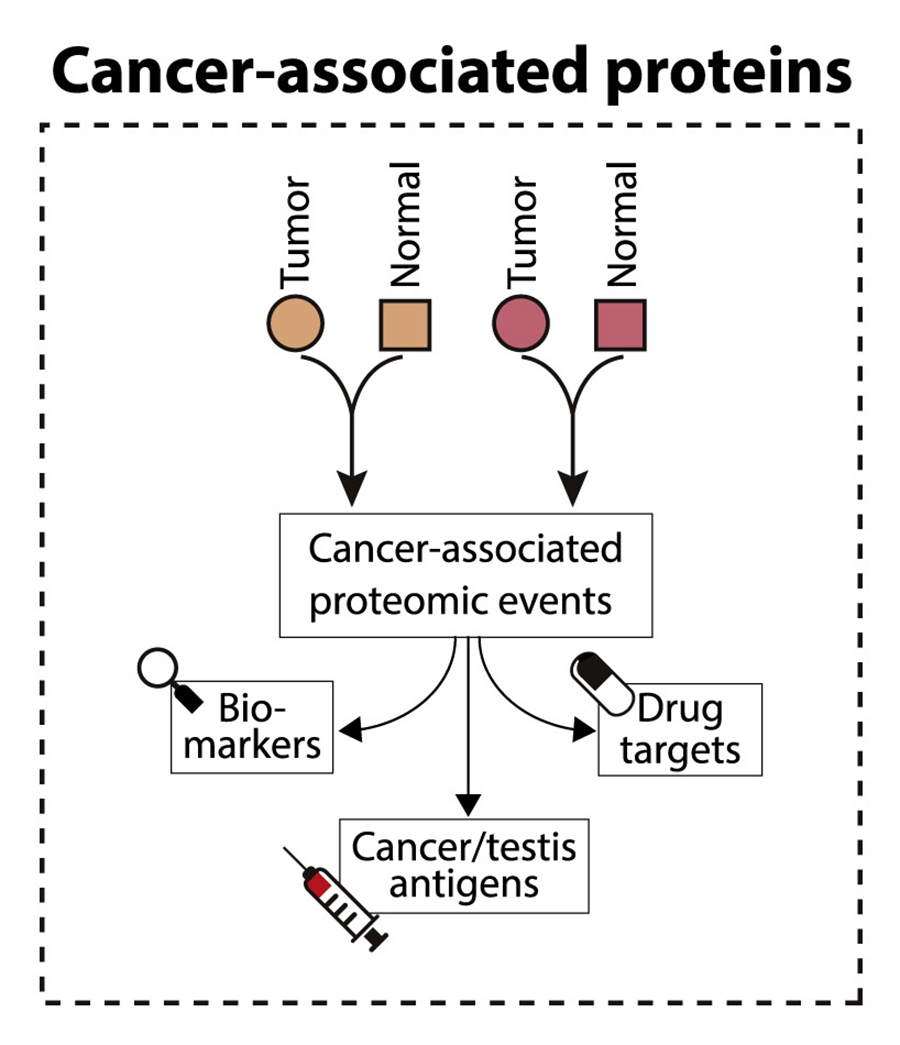
The integrated study of genes and proteins, called proteogenomics, is a fairly new area of research intended to provide researchers with a greater understanding of biology—one that cannot be gained by studying genes alone.
The scientists scoured the gene and protein “profiles” of colon tumors from more than 100 people, identifying several proteins that appear to drive colon cancer growth and could be potential drug targets.
The study, published May 2 in Cell, was led by members of NCI’s Clinical Proteomic Tumor Analysis Consortium (CPTAC), a collaborative effort to “discover major cancer-causing proteogenomic alterations” in several cancer types, said Henry Rodriguez, Ph.D., director of NCI’s Office of Cancer Clinical Proteomics Research.
In 2014, the CPTAC team completed the first large-scale proteogenomic study of colon cancer, which zeroed in on the basic characteristics of colon tumors.
“A major focus of this new study was: Can we use proteogenomic integration to guide therapies?” said lead investigator Bing Zhang, Ph.D., of Baylor College of Medicine in Houston.
Why Study Proteins?
There’s no doubt that studying genes has revealed a trove of information about cancer biology. For example, scientists have used genetic data from tumors to predict how DNAchanges may affect cancer cell behavior, such as uncontrolled growth.
But DNA gives rise to RNA, which then generates proteins, and proteins are what actually drive cell behavior, Dr. Zhang noted.
One important caveat of genetic studies is that the jump from genetic data to cell behavior isn’t always straightforward because “genetic mutations do not always result in the predicted change in the corresponding protein,” Dr. Rodriguez explained. “And there are many other factors that influence protein activity and contribute to tumor behavior.”
In addition, studies have found that DNA and RNA data are not “sufficient, on their own, to dictate the optimal choice of anti-cancer agents with which to treat a particular patient’s tumor in most cases,” wrote Jung-Kuei Chen, Ph.D., and Michael Yaffe, M.D., Ph.D., of the Koch Institute for Integrative Cancer Research at MIT in an accompanying commentary in Cell.
What’s more, the vast majority of cancer drugs target proteins, not genes, Dr. Zhang noted, so protein studies may be best suited to identify new drug targets.
But until recently, large-scale protein studies (called proteomic studies) had not been possible because “proteomic technology lagged behind genomic technology,” he explained.
CPTAC was formed in 2011 to apply new advances in technology and computational approaches to the study of cancer. Based on the success of CPTAC’s pilot studies, the initiative was later expanded. “This new study is a result of that expansion,” Dr. Rodriguez said.
A New Understanding of Colon Cancer
The CPTAC team began by collecting samples of blood, tumor tissue, and nearby normal tissue from 110 people with colon cancer.
They then captured the sequences of all DNA, RNA, microRNA, and protein molecules in each sample. In addition, they looked at how many copies of each gene were present (gene copy number), the relative amounts of each protein (protein expression), and whether the proteins were chemically modified (protein phosphorylation).
After using computational approaches to merge these data, the team compared the “molecular profiles” of the participants’ tumor tissue with that of their healthy tissue.
Although they identified thousands of differences, certain findings jumped out.
For example, a protein called RB1 is known to keep cell growth in check. The gene for RB1 tends to be deleted in many cancer types, but colon tumors often have more copies of the gene than normal. Why colon cancer cells would have more of a protein that prevents cell growth has baffled scientists for years.
When the CPTAC researchers analyzed their data, an answer became clear: In these colon cancer samples, the RB1 protein was chemically modified in a way that stopped it from controlling cell growth. The data also suggested that this modified RB1 may block a type of cell suicide, called apoptosis, providing another advantage to cancer cells.
What’s more, the team found evidence that an enzyme named CDK2 was likely responsible for chemically modifying RB1. Because drugs that block CDK2 activity are already available, it’s possible that such drugs could work for people with colon cancer, the authors noted.
An Idea to Improve Immunotherapy
The investigators made another interesting finding regarding a subtype of colon cancer called microsatellite instability high (MSI-H). About 20% of people with colon cancer have MSI-H tumors.
The immunotherapy drug pembrolizumab (Keytruda) is approved by the Food and Drug Administration to treat some patients with MSI-H colon cancer, but it doesn’t work for about 60% of such patients and scientists have been trying to understand why.
The team found that, compared with tumors that were not MSI-H, some MSI-H colon tumors had higher amounts of enzymes that control glycolysis, a method that cells use to create energy. What’s more, MSI-H tumors with high levels of those enzymes had very few cancer-killing immune cells. Without immune cells in the tumor, an immunotherapy is not likely to work, Dr. Zhang explained.
This surprising relationship between glycolysis and immune cells raises the possibility of a new approach for patients with MSI-H colon cancer that is immunotherapy-resistant, the authors stated.
More to Explore
While the CPTAC team has found some interesting connections, there’s still a mountain of data to explore, Dr. Zhang pointed out.
This study “presents several clearly testable hypotheses and serves as a valuable colon cancer resource for further focused interrogation,” Drs. Chen and Yaffe wrote.
To enable future investigations, data from this and other CPTAC studies are available to the public for free (subject to a data use agreement), Dr. Rodriguez explained. In fact, more than 19,000 people have used the database to date.
Sharing data “allows a wider group of scientists to replicate [CPTAC’s findings] and, importantly, extend and accelerate research in unanticipated directions,” he said.
And colon cancer isn’t CPTAC’s only focus. They’ve also completed proteogenomic studies of breast, ovarian, endometrial, and kidney cancer and plan to finish studies of three additional cancer types in the coming years, Dr. Rodriguez noted.
If that seems like a lot of work, that’s because it is.
“The teamwork [within CPTAC] is what makes this happen,” Dr. Zhang emphasized. “The power of this consortium is that it brings investigators with expertise in different areas together to address challenging questions,” he added.
































No hay comentarios:
Publicar un comentario