
What is Hematopoiesis?
Hematopoiesis the process through which all cellular components of blood are produced. On an average, a healthy human adult has a blood volume of five litres, which carries out a plethora of essential functions within the body, including the transport of oxygen and nutrients as well as the removal of waste.
Razvan Dan Paun | Shutterstock
Blood plasma
Blood plasma makes up the majority of the total blood volume and contains the following:
- Fibrinogen–when tissue or vascular damage occurs, these glycoproteins facilitate the production of fibrin (a non-globular protein) clots
- Serum albumin–implicated in the maintenance of osmotic pressure between the blood vessels and tissues, this type of protein is also a carrier of antithrombin and heparin cofactor (proteins needed for blood clotting)
- Electrolytes – there are variety of electrolytes in the blood plasma, including chloride, potassium and sodium.
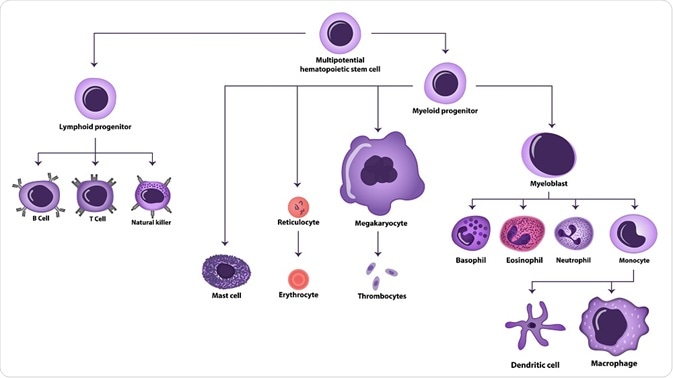
Haematopoiesis is the process by which erythrocytes (red blood cells), lymphocytes, granulocytes, monocytes (types of white blood cells), and thrombocytes (platelets) are produced in the human blood.
What are hematopoietic stem cells?
Hematopoietic stem cells (HSCs) are multipotent cells with the capacity for self-renewal. They differentiate and give rise to the various types of blood cells found in the human body. HSCs express the cell surface glycoprotein CD34, a cell-cell adhesion molecule that is lost from mature blood cells. Haematopoiesis occurs in the yolk sac in the first few weeks of gestation and erythrocytes are the first type of blood cell to be produced.
Location
Primitive erythroid cells can be found in the yolk sac between weeks 2 and 8 of gestation. From the second month of a pregnancy to the seventh month, the liver and spleen are the main hematopoietic sites. Some haematopoiesis occurs in the bone marrow post fifth month of gestation.
HSCs can be found in umbilical cord blood, bone marrow or peripheral blood. However, the HSCs found in umbilical cord blood have greater proliferative response to cytokines due to their primitive nature.
Lifespan
When HSCs divide initially, it gives rise to two daughters cells– HSCs with various cell fates and hematopoietic progenitor cell (HPC) which is limited to one or more differentiation pathways. While blood cells have a finite lifespan, haematopoiesis is required throughout life span.
The Common Myeloid Progenitor Cell
The common myeloid progenitor cell (CFU-GEMM) is able to differentiate into erythrocytes, thrombocytes, lymphocytes, granulocytes, and monocytes. Interleukin-3 and GM-CSF are implicated in the differentiation and proliferation of CFU-GEMM from HPCs.
A cytokine known as Stem cell factor (SCF) can stimulate the growth and total number of CFU-GEMM. CFU-GEMM is the precursor to a variety of colony forming units which ultimately give rise to different blast cells. These include the following:
- CFU-Meg (from which promegakaryoblasts are derived)
- CFU-E (from which proerythroblasts are derived)
- CFU-GM (both monoblasts and myeloblasts are derived from this type of colony forming unit)
extender_01 | Shutterstock
Thrombopoiesis
Thrombocytes are formed by fragmentation of large megakaryocytes, and have an abundance of cytoplasmic granules and lobulated nucle. They are implicated in blood clotting and have an average diameter of 2–4 μm.
Megakaryocytes reside primarily in the bone marrow and play a key role in hemostasis and thrombosis. The production of megakaryocytes is regulated by thrombopoietin (TPO), interleukin-3 (IL-3) and an hematopoietic cytokine called stem cell factor (SCF). TPO is also regulates thrombocyte production.
Erythropoiesis
Oxygen delivery to the tissues is a vital process in the human body. As erythrocytes have finite lifespan (approximately 120 days), the process of erythropoiesis maintains normal levels of erythrocytes in circulation. The first stage of erythroid maturation is the formation of proerythroblasts.
These cells are highly basophilic, have organelles and nuclei which do not contain haemoglobin. They give rise to normoblasts which have small, dense nuclei. When the nucleus is expelled form a normoblast, a reticulocyte is formed. Finally, differentiation produces mature erythrocytes, which have no organelles. At the stage haem production also stops.
Granulopoiesis
Myeloblasts are the precursors to granulocytes. As they develop, cytoplasmic granules are called promyelocytes. Neutrophils, eosinophils and basophils are produced as promyelocytes differentiate along three different pathways. Each subset of granulocyte is characterised by granules specific to their cell type.
Monopoiesis
Monocytes play important roles in cytokine production, phagocytosis, and antigen presentation. The first cell type in the monocytic pathway is the monoblast. As the process of maturation progresses, these precursory cells reduce in size and develop indented nuclei giving rise to promonocytes and eventually, monocytes.
Lymphopoiesis
A diverse range of lymphocytes are produced through lymphopoiesis. B-cells, T-cells, and natural killer cells are produced through this pathway and have a common lymphoid progenitor. Upon leaving the bone marrow, B-cells and T-cells are not mature. Further maturation takes place in the thymus and spleen.
Sources
Further Reading
Last Updated: Nov 19, 2018

































No hay comentarios:
Publicar un comentario