
What is Alzheimer’s Disease?
- The most common type of dementia.
- A progressive disease beginning with mild memory loss possibly leading to loss of the ability to carry on a conversation and respond to the environment.
- Involves parts of the brain that control thought, memory, and language.
- Can seriously affect a person’s ability to carry out daily activities.
Although scientists are learning more every day, right now, they still do not know what causes Alzheimer’s disease.
Who has Alzheimer’s Disease?
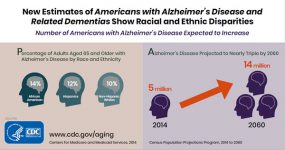
- In 2013, as many as 5 million Americans were living with Alzheimer’s disease.1
- The symptoms of the disease can first appear after age 60 and the risk increases with age.
- Younger people may get Alzheimer’s disease, but it is less common.
- The number of people living with the disease doubles every 5 years beyond age 65.
- By 2050, this number is projected to rise to 14 million people, a nearly three-fold increase.1
What is known about Alzheimer’s Disease?
Scientists do not yet fully understand what causes Alzheimer’s disease. There probably is not one single cause, but several factors that affect each person differently.
- Age is the best known risk factor for Alzheimer’s disease.
- Family history—researchers believe that genetics may play a role in developing Alzheimer’s disease.
- Changes in the brain can begin years before the first symptoms appear.
- Researchers are studying whether education, diet, and environment play a role in developing Alzheimer’s disease.
- Scientists are finding more evidence that some of the risk factors for heart disease and stroke, such as high blood pressure and high cholesterol may also increase the risk of Alzheimer’s
 disease.
disease. - There is growing evidence that physical, mental, and social activities may reduce the risk of Alzheimer’s disease.
How do I know if it’s Alzheimer’s disease?
Alzheimer’s disease is not a normal part of aging.
Memory problems are typically one of the first warning signs of cognitive loss.
According to the National Institute on Aging, in addition to memory problems, someone with Alzheimer’s disease may experience one or more of the following signs:

- Memory loss that disrupts daily life, such as getting lost in a familiar place or repeating questions.
- Trouble handling money and paying bills.
- Difficulty completing familiar tasks at home, at work or at leisure.
- Decreased or poor judgment.
- Misplaces things and being unable to retrace steps to find them.
- Changes in mood, personality, or behavioral.
If you or someone you know has several or even most of the signs listed above, it does not mean that you or they have Alzheimer’s disease. It is important to consult a health care provider when
you or someone you know has concerns about memory loss, thinking skills, or behavioral changes.
- Some causes for symptoms, such as depression and drug interactions, are reversible. However, they can be serious and should be identified and treated by a health care provider as soon as possible.
- Early and accurate diagnosis provides opportunities for you and your family to consider or review financial planning, develop advance directives, enroll in clinical trials, and anticipate care needs.
How is Alzheimer’s disease treated?

Medical management can improve the quality of life for individuals living with Alzheimer’s disease and their caregivers. There is currently no known cure for Alzheimer’s disease.
Treatment addresses several different areas:
- Helping people maintain mental function.
- Managing behavioral symptoms.
- Slowing or delaying the symptoms of the disease.
Support for family and friends

Currently, many people living with Alzheimer’s disease are cared for at home by family members.
Caregiving can have positive aspects for the caregiver as well as the person being cared for. It may bring personal fulfillment to the caregiver, such as satisfaction from helping a family member or friend, and lead to the development of new skills and improved family relationships.
Although most people willingly provide care to their loved ones and friends, caring for a person with Alzheimer’s disease at home can be a difficult task and might become overwhelming at times. Each day brings new challenges as the caregiver copes with changing levels of ability and new patterns of behavior. As the disease gets worse, people living with Alzheimer’s disease often need more intensive care.
You can find more information about caregiving here.
What is the burden of Alzheimer’s disease in the United States?
Alzheimer’s disease is
- One of the top 10 leading causes of death in the United States.2
- The 6th leading cause of death among US adults.
- The 5th leading cause of death among adults aged 65 years or older.3
In 2013, an estimated 5 million Americans aged 65 years or older had Alzheimer’s disease.1 This number may triple to as high as 13.8 million people by 2050.1
In 2010, the costs of treating Alzheimer’s disease were projected to fall between $159 and $215 billion.4 By 2040, these costs are projected to jump to between $379 and more than $500 billion annually.4
Death rates for Alzheimer’s disease are increasing, unlike heart disease and cancer death rates that are on the decline.5 Dementia, including Alzheimer’s disease, has been shown to be underreported in death certificates and therefore the proportion of older people who die from Alzheimer’s may be considerably higher.6
Alzheimer’s Disease Public Health Curriculum
A Public Health Approach to Alzheimer’s and Other Dementias is an introductory curriculum that is intended to increase awareness of the impact of Alzheimer’s disease and other dementias as well as the role of public health. This curriculum addresses cognitive health, cognitive impairment, and Alzheimer’s disease and is intended for use by undergraduate faculty in schools and programs of public health and other related disciplines. This work supports The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships (Road Map) in its goal of developing a competent workforce. The curriculum is available free of charge and consists of four modules that are designed to be used individually or as a whole each with slides and a faculty guide.
| Module | Description | Faculty Guide | Slides |
|---|---|---|---|
| Course Overview | Provides an overview of each module with learning objectives. | View[PDF – 530 KB] | |
| Module 1: Alzheimer’s Disease – A Public Health Crisis | Alzheimer’s and other dementias are framed as a public health epidemic with a large and rapidly growing burden that bears significant impact on the nation. | View[PDF – 4 MB] | View[PPT – 3 MB] View[PDF – 2 MB] |
| Module 2: Alzheimer’s and Other Dementias – The Basics | Alzheimer’s and other dementias are described including symptoms, stages, risk factors, diagnosis, and management. | View[PDF – 3 MB] | View[PPT – 4 MB] View[PDF – 2 MB] |
| Module 3: Alzheimer’s Disease – What is the Role of Public Health? | Three tools of public health that may play a significant role in mitigating the Alzheimer’s disease epidemic are discussed: surveillance/monitoring, primary prevention, and early detection and diagnosis. | View[PDF – 3 MB] | View[PPT – 4 MB] View[PDF – 2 MB] |
| Module 4: Dementia Capable Systems and Dementia Friendly Communities | The public health response to the Alzheimer’s disease epidemic on a state and community level is addressed. The module describes the concept of a “dementia capable” system and explores how public health may support the development of such systems through public health research and translation, support services and programs, workforce training, and the creation of dementia-friendly communities. | View[PDF – 3 MB] | View[PPT – 11 MB] View[PDF – 2 MB] |
| Complete Course | An introductory curriculum that is intended to increase awareness of the impact of Alzheimer’s and other dementias as well as the role of public health. | View[PDF – 10 MB] | |
| About the Curriculum | Curricular materials developed on cognitive health, cognitive impairment, and Alzheimer’s disease for use by undergraduate faculty in schools and programs of public health. | View[PDF – 578 KB] | |
| References | Provides the references and supporting material for the curriculum content. | View[PDF – 624 KB] |
Resources on Aging, Alzheimer's Disease and Cognitive Health
Aging
- CDC Healthy Aging Program
- National Institute on Aging
- The National Library of Medicine
- Administration for Community Living
CDC Healthy Brain Initiative
- The Healthy Brain Initiative
- The Healthy Brain Initiative: A National Public Health Road Map to Maintaining Cognitive Health
Other Alzheimer’s Disease and Cognitive Health Resources
References
- Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-83.
- Xu J, Kochanek KD, Sherry L, Murphy BS, Tejada-Vera B. Deaths: final data for 2007. National vital statistics reports; vol. 58, no. 19. Hyattsville, MD: National Center for Health Statistics. 2010.
- Heron M. Deaths: leading causes for 2010. National vital statistics reports; vol. 62, no 6. Hyattsville, MD: National Center for Health Statistics. 2013.
- Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. NEJM. 2013;368(14):1326-34.
- Tejada-Vera B. Mortality from Alzheimer’s disease in the United States: data for 2000 and 2010. NCHS data brief, no 116. Hyattsville, MD: National Center for Health Statistics. 2013.
- James BD. Leurgans SE, Hebert LE, et al. Contribution of Alzheimer disease to mortality in the United States. Neurology. 2014;82:1-6.





















.png)










No hay comentarios:
Publicar un comentario