
Why are Women More Likely to have Brain Aneurysms Compared to Men?
A brain aneurysm is a diseased or abnormal dilatation of the cerebral arteries at a weak spot. These typically thin-walled aneurysmal sacs of blood may continue to enlarge because of the force of the arterial pulsatile flow. A ruptured aneurysm leads to a subarachnoid hemorrhage, an SAH.
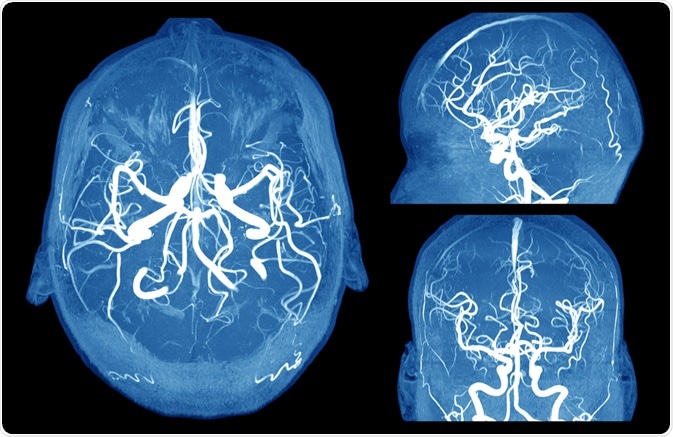
Image Credit: MriMan/Shutterstock.com
Skewed Gender Representation in Aneurysm Formation
Worldwide, cerebral aneurysms occur in 3.2% of the global population, with the mean age of presentation being 50 years. Scientists estimate that over 6 million Americans have an unruptured aneurysm in the brain, and about 30,000 of them rupture each year. In 40 of each hundred ruptures, the patient dies.
Brain aneurysms are more common in females by about 60% overall, and more especially in the postmenopausal age group, where the risk is more than twice as high.
This has prompted the hypothesis that sex hormones are involved in the formation of aneurysms. This may be the reason, some say, that women are protected against aneurysms in their reproductive years, but the incidence rises after menopause.
Apart from the prevalence, there is a clear gender difference in the anatomical location and the time of presentation of the cerebral aneurysm. While men have more aneurysms (ruptured and unruptured) in the anterior cerebral circulation, women tend to have more along the internal carotid artery, for reasons that are not clear.
The average age of men presenting with aneurysms is a few years younger than that of women with the same presentation. Moreover, women tend to have multiple aneurysms more often than men do.
Women are also possibly at a greater risk of rupture of aneurysms, though all studies do not agree on this finding.
Why Do Aneurysms Form?
it is important to understand the process of aneurysm formation because alterations in this process may be responsible for the increased representation in women.
Hemodynamic stress occurs due to the turbulent flow of blood along the brain’s blood vessels. The vibrations of turbulent flow and the collagen weakening cause the internal elastic lamina of the artery to weaken over time.
In addition, inflammation mediated by the T lymphocytes and macrophages may cause the collagen to break down. All these factors work together to prompt the formation and growth of an aneurysm. There are other risk factors like smoking and possibly hypertension, which exacerbate this risk.
Why Are Females More Susceptible to Brain Aneurysms?
Several mechanisms have been put forward to explain why females should be more vulnerable to the formation of cerebral aneurysms.
Estrogen receptors
The brain circulation is regulated via multiple mechanisms, including the pH, the pCO2, nerve impulses, and metabolic factors, but estrogen has a marked effect as well.
Estrogen effects are thought to be mediated by receptors. In female rats, the cerebral blood vessels show a wealth of estrogen receptors alpha (ER-α) on both the smooth muscle and the endothelium cells.
Estrogen affects vascular responses in the brain, as well as the levels of endothelial nitric oxide synthase (eNOS), and prostacyclin synthase. These are enzymes involved in the production of the vasodilator compounds nitric oxide (NO) and prostacyclin.
Knockout mice (without these receptors) do not have an increase in these enzymes even if they are treated with estrogen. In the presence of an estrogen receptor antagonist, the vascular tissue of female rats fails to show an increase in eNOS even with estrogen movement.
Different forms of the ER-α have been found. In the rat study, removal of the ovary reduced all ER forms, but their expression was enhanced after the rats were exposed to estrogen for a long period. This suggests that estrogen has a protective effect on the cerebral blood vessels.
The higher level of ER-α following chronic estrogen exposure could be a reserve; one way to ensure that estrogen can produce changes in the enzyme levels that increase vasodilator concentrations, despite the fact that these receptors are constantly undergoing a turnover by proteasomal degradation.
Reduced Collagen Content
The first theory is that the arteries of the brain are weaker in older women because of reduced estrogen stimulation after menopause. This may reduce the collagen content in the vessel wall.
Endothelial factors
In other studies of vasocontraction carried out on rat and mouse cerebral arteries, the effects of chronic estrogen occurred only if the endothelium was intact.
In other words, estrogen influences the contractile activity of the blood vessel through the endothelium rather than by any direct effect on the smooth muscle of the arterial wall.
Genomic action
The mechanism of estrogen action is thought to include the classic genomic effect, whereby the hormone binds to nuclear receptors to induce transcription, thereby activating specific genes.
However, there is also a suggestion that nongenomic effects occur because certain changes are too rapid to have been brought about by the genomic mechanism.
For instance, endothelial cells in culture show immediate NO production and release as well as activation of the mitogen-activated protein kinase (MAPK) pathway on exposure to estrogen. This was inhibited by estrogen receptor antagonists.
Altered hemodynamics
Hormonal influences are not the only explanation, however. Other influences include vessel wall weakness and stress due to the flow of blood.
Hemodynamic forces could induce the formation of aneurysms by increasing wall shear stress (WSS). This could damage the endothelial lining, inducing remodeling changes in the vascular endothelium.
One study shows that women have measurably smaller diameters in the brain blood vessels. As a result, blood flow is faster and WSS higher at the forks of the middle cerebral artery (MCA) and even more, the internal carotid artery (ICA).
Simulations of blood flow have shown that smaller vessels which branch more asymmetrically have higher peak pressures and increased WSS.
The higher WSS in women could put them at higher risk of aneurysms along the ICA course. Even at the same blood pressure, therefore, the reduced vessel diameter in women relative to men in the proximal part of the ICA increases the chances of aneurysm formation in women.
The size ratio, that is, the ratio of intracranial aneurysm diameter to vessel diameter increases the risk of rupture. Since women tend to have smaller blood vessel diameter, this increases their risk of aneurysmal rupture.
Independent risk factors
The classic risk factors for aneurysm formation in both men and women include smoking, hypertension, and alcoholism. In women, these may increase the risk of having a SAH due to aneurysmal rupture. A history of a ruptured aneurysm in an immediate family member is another high-risk factor.
Most aneurysms occur between the ages of 35 and 60 but can exist above or below these limits. If a woman has any of the above risk factors, it is advised that she quit smoking, drink less, bring her blood pressure under control and be watchful for symptoms of aneurysm enlargement.

Image Credit: Voyagerix/Shutterstock.com
Should aneurysms always be treated?
It is estimated that 3% to 5% of Americans have brain aneurysms over their lifetimes, but only about 30,000 of them come to medical attention because of rupture. About half the patients with a rupture die immediately or within 6 months.
However, the scientific consensus is against treating incidentally detected aneurysms, in most cases, because of the high risk associated with surgical management.
New models are being developed to help predict the risk of rupture and thus decide on further management, using non-invasive imaging tools.
Scientists are also investigating the role of low-dose aspirin in the prevention of these aneurysms, and the use of coils and other materials to block them simply and effectively.
References and Further Reading
- Stirone, C., Duckles, S. P., and Krause, D. N. (2002) Multiple forms Of Estrogen Receptor-α In Cerebral Blood Vessels: Regulation by Estrogen. American Journal of Physioogy. https://doi.org/10.1152/ajpendo.00165.2002. https://journals.physiology.org/doi/full/10.1152/ajpendo.00165.2002
- Harrod, C. G., Batjer, H. H., and Bendok, B. R. (2005) (Deficiencies in Estrogen-Mediated Regulation of Cerebrovascular Homeostasis May Contribute to An Increased Risk of Cerebral Aneurysm Pathogenesis and Rupture In Menopausal And Postmenopausal Women. Medical Hypotheses 2006;66(4):736-56. Epub 2005 Dec 13. https://doi.org/10.1016/j.mehy.2005.09.051. https://www.ncbi.nlm.nih.gov/pubmed/16356655/
- Júnior, J. R., Telles, J. P., da Silva S. A. et al. (2019). Epidemiological Analysis Of 1404 Patients with Intracranial Aneurysm Followed in A Single Brazilian Institution. Surgical Neurology International 10:249. https://dx.doi.org/10.25259%2FSNI_443_2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935967/
- Turan, N., Heider, R. A., Zaharieva, D., Ahmad, F. U., et al. (2016). Sex Differences in the Formation of Intracranial Aneurysms and Incidence and Outcome of Subarachnoid Hemorrhage: Review of Experimental and Human Studies. Translational Stroke Research. 2016 Feb;7(1):12-9. doi: 10.1007/s12975-015-0434-6. Epub 2015 Nov 16. https://www.ncbi.nlm.nih.gov/pubmed/26573918
- Ghods, A. J., Lopes, D., and Chen, M. (2012). Gender Differences in Cerebral Aneurysm Location. Frontiers in Neurology. 2012; 3: 78. Published online 2012 May 21. doi: 10.3389/fneur.2012.00078. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3356859/
- Jersey, A. M., and Foster, D. M. (2019). Cerebral Aneurysm. [Updated 2019 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507902/
- Nih.gov. (2020). Cerebral Aneurysms Fact Sheet. Available at: https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/cerebral-aneurysms-fact-sheet. (Accessed on 27 April 2020).
Further Reading
Last Updated: May 4, 2020

































No hay comentarios:
Publicar un comentario