

Midostaurin Approved by FDA for Acute Myeloid Leukemia
June 1, 2017, by NCI Staff
On April 28, the Food and Drug Administration (FDA) approved the addition of the targeted therapy midostaurin (Rydapt®) for adults receiving chemotherapy for newly diagnosed acute myeloid leukemia (AML) with certain mutations in the FLT3 gene. Approximately 25% to 30% of AML cases carry FLT3 mutations, and these mutations are associated with a particularly aggressive form of the disease.
The approval of midostaurin for AML requires the use of the LeukoStrat CDx FLT3 Mutation Assay, a companion diagnostic test FDA also approved for detecting FLT3 mutations.
The approval of midostaurin for AML requires the use of the LeukoStrat CDx FLT3 Mutation Assay, a companion diagnostic test FDA also approved for detecting FLT3 mutations.
The international phase III clinical trial on which the approval was based was a collaboration between the NCI-sponsored Alliance for Clinical Trials in Oncology and Novartis, which manufactures midostaurin. The Alliance provided the infrastructure for FLT3 mutation testing in the United States and worldwide data management for the clinical trial.
“This is the first advance in AML in decades,” commented Richard Little, M.D., of NCI's Division of Cancer Treatment and Diagnosis. “It really illustrates the importance of approaching AML not as one disease but as a variety of diseases [based on genetics] that can be identified and targeted in clinical trials.”
“This is the first advance in AML in decades,” commented Richard Little, M.D., of NCI's Division of Cancer Treatment and Diagnosis. “It really illustrates the importance of approaching AML not as one disease but as a variety of diseases [based on genetics] that can be identified and targeted in clinical trials.”
FDA also approved the use of midostaurin for the treatment of adults with aggressive systemic mastocytosis (SM; a condition in which there are too many mast cells in the body), SM with associated hematologic neoplasm, and mast cell leukemia—all rare diseases with a poor prognosis.
Targeted Therapy Improves Survival
Data from the randomized double-blind, placebo-controlled trial of midostaurin for AML were presented at the 2015 meeting of the American Society of Hematology.
In that trial, 717 patients aged 18 to 60 with newly diagnosed FLT3 mutation–positive AML were randomly assigned to receive midostaurin plus standard chemotherapy, consisting of the drugs daunorubicin (Cerubidine®) and cytarabine (Cytosar-U®), or placebo plus standard chemotherapy.
In that trial, 717 patients aged 18 to 60 with newly diagnosed FLT3 mutation–positive AML were randomly assigned to receive midostaurin plus standard chemotherapy, consisting of the drugs daunorubicin (Cerubidine®) and cytarabine (Cytosar-U®), or placebo plus standard chemotherapy.
Patients in both treatment groups could receive a stem-cell transplant as part of their therapy if their doctors determined they needed one. A similar number of patients in both groups received a stem cell transplant, and the median time to transplant was also similar.
Midostaurin decreased the risk of death by 23% compared with placebo. The percentage of patients alive 5 years after diagnosis was 50.9% in the midostaurin group compared with 43.9% in the placebo group.
The number of serious adverse events was also similar in the two treatment groups. Febrile neutropenia (a condition marked by fever and a lower-than-normal number of a kind of white blood cell) occurred in 16% of patients in both groups, and was the most common serious adverse event in the trial. Other common side effects included nausea, mucositis, vomiting, headache, petechiae, and musculoskeletal pain.
While these results are exciting for patients with FLT3 mutation–positive AML, “the effect size in this trial was relatively modest,” said Dr. Little. “We’d like to see an agent that could benefit more patients than we saw in this trial.”
NCI, through its National Clinical Trials Network, is planning trials of newer targeted therapies in AML that are collaborative in design like the midostaurin trial, he explained.
“This sort of international collaboration for a rare disease is a good example of an [effective] public–private partnership,” he said.
Midostaurin decreased the risk of death by 23% compared with placebo. The percentage of patients alive 5 years after diagnosis was 50.9% in the midostaurin group compared with 43.9% in the placebo group.
The number of serious adverse events was also similar in the two treatment groups. Febrile neutropenia (a condition marked by fever and a lower-than-normal number of a kind of white blood cell) occurred in 16% of patients in both groups, and was the most common serious adverse event in the trial. Other common side effects included nausea, mucositis, vomiting, headache, petechiae, and musculoskeletal pain.
While these results are exciting for patients with FLT3 mutation–positive AML, “the effect size in this trial was relatively modest,” said Dr. Little. “We’d like to see an agent that could benefit more patients than we saw in this trial.”
NCI, through its National Clinical Trials Network, is planning trials of newer targeted therapies in AML that are collaborative in design like the midostaurin trial, he explained.
“This sort of international collaboration for a rare disease is a good example of an [effective] public–private partnership,” he said.
Efficacy in an Even Rarer Disease
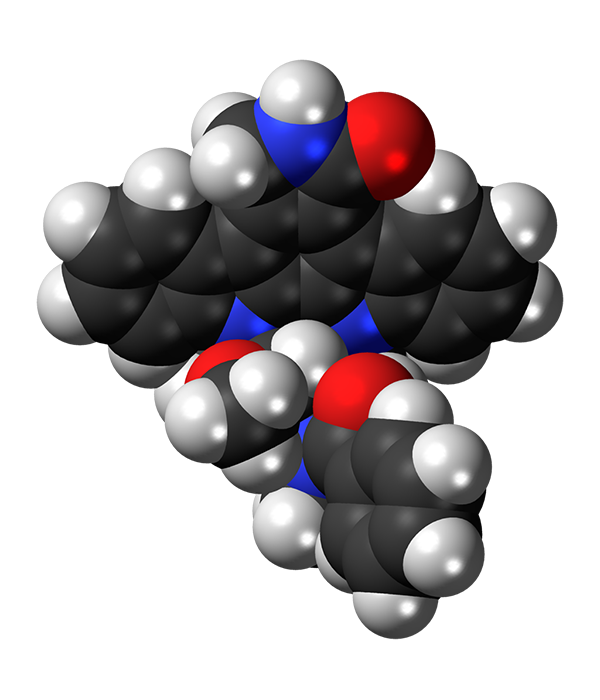
Midostaurin belongs to a class of drugs called multi-kinase inhibitors, which can target more than one protein in cells. While in AML that target is FLT3, in aggressive SM and related conditions the target is a mutant protein called KIT D816V, which is found in about 90% of mastocytosis cases.
In a single-arm clinical trial that led to FDA’s approval of midostaurin for SM and related conditions, funded by Novartis, 116 patients received midostaurin as a single therapy. Of these, 89 patients already had organ damage from their disease.
Overall, 60% of patients with organ damage responded to the drug, with 45% having what the trial investigators classified as a major response: the complete resolution of at least one type of organ damage caused by mastocytosis. Trial participants had a median overall survival of 33.9 months, and the 16 patients in the trial with mast cell leukemia had a median overall survival of 9.4 months. Historically, median overall survival with mast cell leukemia has been less than 6 months.
More than half of patients required a dose reduction during treatment due to side effects, which included a drop in blood count, nausea, vomiting, and diarrhea; however, about one-third of these dose reductions were temporary.
In a single-arm clinical trial that led to FDA’s approval of midostaurin for SM and related conditions, funded by Novartis, 116 patients received midostaurin as a single therapy. Of these, 89 patients already had organ damage from their disease.
Overall, 60% of patients with organ damage responded to the drug, with 45% having what the trial investigators classified as a major response: the complete resolution of at least one type of organ damage caused by mastocytosis. Trial participants had a median overall survival of 33.9 months, and the 16 patients in the trial with mast cell leukemia had a median overall survival of 9.4 months. Historically, median overall survival with mast cell leukemia has been less than 6 months.
More than half of patients required a dose reduction during treatment due to side effects, which included a drop in blood count, nausea, vomiting, and diarrhea; however, about one-third of these dose reductions were temporary.
“Mastocytosis is a much less common disease [than AML], and this is a much welcome advance in that disease as well,” concluded Dr. Little.





















.jpg)










No hay comentarios:
Publicar un comentario