
No symptoms? No thyroid testing!
The Canadian Task Force on Preventive Health Care has published new recommendations that rule out the need to do a thyroid screening test “just because” if the patient doesn’t have symptoms of thyroid abnormality, is an adult, isn’t pregnant, and has no risk factors for thyroid disease. This should put to rest any doubts that thyroid screening is a part of a routine check-up. The guideline was issued after a strictly performed systematic review and published in the Canadian Medical Association Journal (CMAJ).
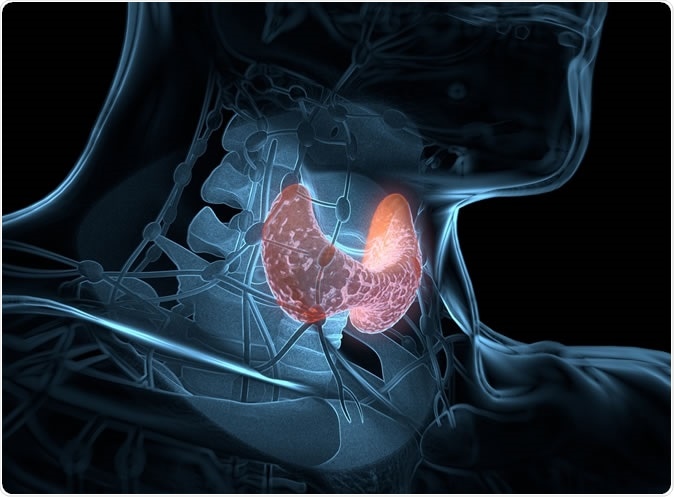
Thyroid gland inside human body. 3D illustration. Credit: Anatomy Insider / Shutterstock
The TSH test
In most cases a routine thyroid test is ordered by doing a thyroid stimulating hormone (TSH) assessment. When TSH levels are low or high, it may indicate an overactive or a sub-functioning thyroid, respectively. In most cases, the physician simply checks the box for TSH on the blood test requisition form.
However, the guideline is directed at just such practitioners, asking them to rethink this test when done as a part of a routine health check-up rather than because the patient has symptoms that trigger suspicion of thyroid disease. Researcher Richard Birtwhistle says, “The evidence isn't there to suggest a health benefit for this type of screening as a routine part of care.”
Thyroid dysfunction – the symptoms
Recapitulating the symptoms of thyroid over- or underactivity, another member of the task force says, “Patients who are unusually tired; sensitive to cold or heat; or experience hair loss, heartbeat irregularities, unexpected weight loss or gain should visit their primary care practitioner." The guideline is intended for those without any such symptoms, or who have had radiation, for instance, to the head and neck, have had medications which reduce thyroid activity, or have disease conditions that affect hypothalamic and pituitary health.
Thyroid overactivity, also called hyperthyroidism, is caused by conditions like Graves’ disease, toxic goiter and toxic adenoma of the thyroid. Hypothyroidism, which refers to a slow sluggish thyroid, is caused by Hashimoto’s thyroiditis, an autoimmune condition, or due to medication. Both are linked to impairment of many physical processes, with hypothyroidism causing complications such as slow thinking, a rise in blood pressure, heart dysfunction, and high blood lipid levels. Hyperthyroidism is more immediately recognizable, producing life-threatening cardiac arrhythmias, bone fractures and even a thyroid storm.
About 10% of Canadians above 45 years have been diagnosed with thyroid dysfunction, but disproportionately more in women (16% of females) compared to men (4%). Especially with milder cases, TSH usually returns to normal over time.
The basis
The guideline is based on 22 studies that evaluated the effectiveness of the common practice of treating adults without symptoms of thyroid disease simply because the routinely-ordered TSH test came up abnormal. The research team says they could not find proof that people actually benefit from either the screening or the treatment, in the absence of symptoms.
And in fact, it could be actually harmful – in the sense that all medication taken unnecessarily is harmful, as is the need to visit a doctor regularly, or to have regular blood checks to monitor the TSH trends. Thus, the committee has come up with a strong healthcare recommendation based on evidence that has low certainty of benefit but high certainty of potential harm or of resource expenditure.
This guideline is endorsed by many other professional and health organizations, such as the British Columbia Ministry of Health, The College of Family Physicians of Canada, Nurse Practitioner Association of Canada and the Canadian Society of Endocrinology and Metabolism, and Toward Optimized Practice from Alberta.
The reasons are varied, but include the lack of any clinical benefit, the cost of running unnecessary tests, and wastage of patient and physician time, as well as the psychological burden of considering oneself sick when one is not. These resources, says Birtwhistle, could be used better elsewhere. Of course, a few specialists disagree, especially when it comes to screening older citizens for undetected thyroid dysfunction.
Implications
Commending the work of the Canadian task force, endocrinologists Omar El Kawkgi and Juan Brito sum up: ” By issuing a strong recommendation against population screening for thyroid dysfunction, the task force may help physicians to stop uncovering a large reservoir of people with mild thyroid dysfunction who are unlikely to benefit from identification or treatment, thereby preventing the overdiagnosis and overtreatment of otherwise healthy people.”
Journal reference:
Recommendation on screening adults for asymptomatic thyroid dysfunction in primary care Richard Birtwhistle, Kate Morissette, James A. Dickinson, Donna L. Reynolds, Marc T. Avey, Francesca Reyes Domingo, Rachel Rodin, Brett D. Thombs CMAJ Nov 2019, 191 (46) E1274-E1280; DOI: 10.1503/cmaj.190395, https://www.cmaj.ca/content/191/46/E1274

































No hay comentarios:
Publicar un comentario