
Researchers Use CRISPR Gene-Editing Tool to Help Turn Immune Cells against Tumors
March 20, 2017, by NCI Staff
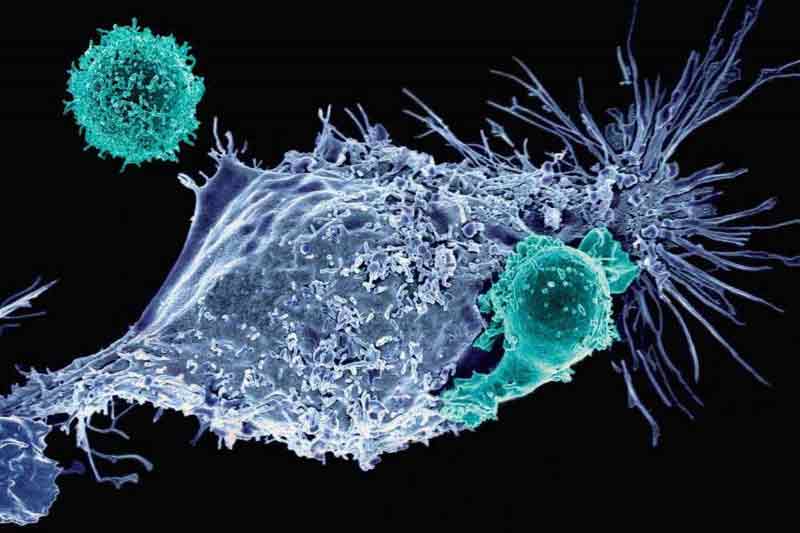
Using a new tool for editing genomes, known as CRISPR, researchers have genetically engineered immune cells and improved the ability of these cells to kill cancer cells in mice.
The cells were modified to express proteins on their surfaces called chimeric antigen receptors (CARs), which enabled the cells to recognize and attack cancer cells that expressed the corresponding antigen.
In experiments with the mice, immune cells that had been engineered to express CARs using CRISPR were more effective at killing tumor cells than immune cells engineered using conventional methods, the researchers reported in Nature on February 22.
The type of immunotherapy evaluated in the study is CAR T-cell therapy, a form of adoptive cell transfer. With this treatment, a patient’s own T cells, a type of immune cell, are collected from blood, modified genetically to make them better at attacking tumor cells, expanded in the laboratory, and finally returned to the patient.
To explore ways to enhance the effectiveness of CAR T-cell therapies, Michel Sadelain, M.D., Ph.D., of Memorial Sloan Kettering Cancer Center, and his colleagues turned to a technique called CRISPR, which allows researchers to edit genomes with more speed and precision than other approaches.
Creating More Potent T Cells
Conventional approaches for engineering T cells to express a CAR, such as using a retrovirus to deliver the gene, result in the gene being inserted at random locations in the genome.
With these approaches, however, there is a chance that the CAR gene could insert itself in a way that disrupts the normal functioning of the genome, causing unintended consequences, the study authors noted.
By contrast, the CRISPR/Cas9 system allows for the specific placement of genes. Dr. Sadelain and his colleagues used CRISPR to deliver a CAR gene to a precise location in the T-cell genome: the T-cell receptor alpha chain (TRAC) gene.
The TRAC region of the genome includes the gene for the T-cell receptor, which helps the immune cell detect foreign molecules. The CRISPR system edits out part of the TRAC gene in the T cells, allowing the CAR gene to insert there.
When the researchers tested the two kinds of CAR T cells in mouse models of leukemia, those in which the CAR gene had been inserted at the TRAC locus via CRISPR were more effective at destroying tumor cells than those in which it was inserted randomly with a retrovirus.
Experiments suggested that the improved anti-tumor responses of cells engineered using CRISPR was the result, in part, of the “highly regulated CAR expression” in these T cells, noted Dr. Sadelain.
Overcoming “Exhaustion”
In addition, the CAR T cells created with CRISPR were less likely to stop recognizing and attacking tumor cells after a certain time point, a phenomenon researchers call “exhaustion.”
“We found that the level of CAR expression [on T cells] and the dynamic response of the CAR following the recognition of antigens are critical in determining whether exhaustion will occur rapidly,” explained Dr. Sadelain. “Expressing the CAR from the TRAC locus greatly diminished exhaustion, resulting in superior tumor eradication.”
Based on three measures of exhaustion, less than 2% of CRISPR-created T cells showed signs of exhaustion, compared with up to half of conventionally engineered CAR T cells.
“This report describing the use of CRISPR/Cas9 technology to insert a CAR gene into a specific location in the genome is an important advance for the CAR field,” said James N. Kochenderfer, M.D., who develops and tests T-cell therapies in NCI’s Center for Cancer Research (CCR) and was not involved in the study.
“The finding that the location of CAR gene insertion can affect T-cell function is particularly intriguing,” Dr. Kochenderfer continued. “New gene-editing technologies will likely lead to rapid improvement in antigen-targeted T-cell immunotherapies for cancer.”
Looking Ahead
In an accompanying editorial, Marcela V. Maus, M.D., Ph.D., of Harvard Medical School identified three important improvements that CRISPR could potentially bring to T-cell-based therapies, one being more-effective tumor responses.
Second, the targeted nature of CRISPR-mediated CAR integration into the genome might “prove safer than random integration, which carries the potential risk of generating a harmful mutation,” Dr. Maus wrote.
Finally, this approach might “enable off-the-shelf CAR T cells to be made that need not come from a patient's own T cells,” she continued. “This would enable easier and cheaper manufacture of CAR T cells.”
At Memorial Sloan Kettering, Dr. Sadelain’s team has been modifying its manufacturing techniques to prepare for clinical testing in the future. The researchers believe their findings could have implications for research on diseases other than cancer.
“The biology of CARs still has many secrets and surprises to reveal,” Dr. Sadelain said, adding: “Research on CARs will lead to more effective and safer therapies for a number of diseases.”





















.jpg)










No hay comentarios:
Publicar un comentario