
Making Health Care Safer
Protect patients from antibiotic resistance
Overview
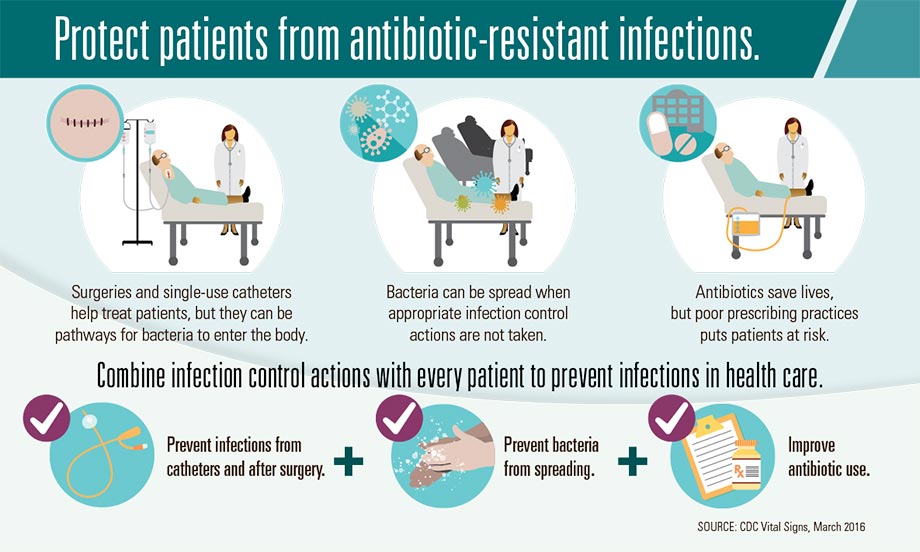
People receiving medical care can get serious infections called healthcare-associated infections (HAIs), which may lead to sepsis or death. Hospitals report common HAIs to CDC, including infections caused by C. difficile, infections following surgery, and infections following placement of a tube in the bladder or a large vein (catheter). These infections can be caused by bacteria that are resistant to antibiotics, making them difficult to treat. In certain kinds of hospitals, one in four of these infections (not including C. difficile) are caused by antibiotic-resistant bacteria identified by CDC as urgent or serious threats to health.* Although progress has been made, more work is needed. Three critical efforts to prevent an HAI are 1) prevent infections related to surgery or placement of a catheter, 2) prevent spread of bacteria between patients, and 3) improve antibiotic use. It’s important that healthcare providers take these actions with every patient every time to prevent HAIs and stop the spread of antibiotic resistance.
Healthcare providers need to:
- Follow recommendations for preventing C. difficile and infections that can occur after surgery or are related to single-use catheters placed in the body. Follow recommended actions with every patient every time. Isolate patients when appropriate, and know antibiotic resistance patterns in your facility/area.
- Prescribe antibiotics correctly. Get cultures, start antibiotics promptly, and reassess 24-48 hours later. Know when to stop antibiotic treatment.
*Long-term acute care hospitals, which provide complex medical care, such as ventilator or
wound care, for long periods of time.
wound care, for long periods of time.

Problem
Antibiotic-resistant HAIs are a threat to all patients.
- HAIs are commonly caused by antibiotic-resistant bacteria, which may lead to sepsis or death. One in seven catheter- and surgery-related HAIs in acute care hospitals, and one in four catheter- and surgery-related HAIs in long-term acute care hospitals, is caused by any of six resistant bacteria (not including C. difficile).
- These six bacteria are among the most deadly antibiotic-resistant bacteria, identified as urgent or serious threats by CDC: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus ), ESBL-producing Enterobacteriaceae (extended-spectrum ß-lactamases), VRE (vancomycin-resistant enterococci), multi-drug resistant pseudomonas, and multi-drug resistant Acinetobacter.
- Progress has been made in preventing HAIs, including a 50% decrease in central line-associated blood stream infections from 2008 to 2014, but more work is needed.
- C. difficile is the most common type of bacteria responsible for infections in hospitals. Most C. difficile is not resistant to the antibiotics used to treat it, but antibiotic use puts patients at high risk for deadly diarrhea.
What Can Be Done
The Federal government is
- Preventing infections and their spread:
Conducting surveillance for HAIs and antibiotic resistance, using data to target prevention, and promoting implementation of recommendations. Identifying emerging resistant threats. Promptly responding to and controlling outbreaks. - Improving antibiotic use:
Promoting appropriate use and providing guidance/assessing implementation of stewardship programs across health care settings. - Promoting use of data:
Preventing HAIs and improving antibiotic use to better protect patients. Collaborating with partners to implement prevention and stewardship strategies, including in federal facilities. www.cdc.gov/hai/surveillance/ar-patient-safety-atlas.html
Healthcare providers need to
- Prevent infections and their spread:
Follow recommendations for preventing C. difficile and infections that can occur after surgery or related to single-use catheters placed in the body. Follow recommended actions with every patient every time. Isolate patients when appropriate, and know antibiotic resistance patterns in your facility/area. - Improve antibiotic use:
Prescribe antibiotics correctly. Get cultures, start antibiotics promptly, and reassess 24-48 hours later. Know when to stop antibiotic treatment.
Health care facility CEOs/ administrators can
- Prevent infections and their spread:
Follow CDC guidelines for preventing infections and promote data use to target prevention and improvements. Make sure staff follow hand hygiene, isolation, and environmental/device cleaning practices. www.cdc.gov/hai/prevent/tap.html - Improve antibiotic use:
Establish stewardship program and enroll your hospital to submit data to CDC’s Antimicrobial Use and Resistance (AUR) Module to target improvements. www.cdc.gov/nhsn/acute-care-hospital/aur/index.html - Prioritize:
Make infection prevention, sepsis prevention, and stewardship a priority; participate in a Quality Innovation Network.
State and local health departments can
- Prevent infections and their spread:
Set goals, monitor your state’s progress in preventing infections, promote action, and achieve regional prevention. Support institutions to meet goals. www.cdc.gov/hai/progress-report - Improve antibiotic use:
Support stewardship efforts and know antibiotic resistance patterns in your area.
Patients and their families can
- Prevent infections and their spread:
If you have a catheter, ask daily if it’s necessary. If you are having surgery, ask your doctor how he/she prevents infections. Insist that everyone clean their hands before touching you. Clean your hands often. Explore Hospital Compare tool for HAI data. https://www.medicare.gov/hospitalcompare/search.html - Improve antibiotic use:
Ask if your antibiotic is necessary and what is being done to improve antibiotic use and protect patients.
























.png)









No hay comentarios:
Publicar un comentario