
The Microbiome & Innovations to Slow Antibiotic Resistance
As part of its continued efforts to protect patients and slow antibiotic resistance, CDC is investing in research to discover and develop new ways to prevent antibiotic-resistant infections and their spread, as well as unlock the mysteries of the microbiome. These efforts support CDC’s Antibiotic Resistance Solutions Initiative and implement the tracking, prevention, and antibiotic stewardship activities outlined in the National Action Plan for Combating Antibiotic-Resistant Bacteria[63 pages]
Applied Microbiome Research to Improve Public Health
CDC is expanding its work in the microbiome to slow antibiotic resistance.
The microbiome is a community of naturally-occurring germs in and on our bodies. Bacteria live naturally on our skin, in our gut, in our mouths or respiratory tracts, and in our urinary tracts.
Antibiotics impact the microbiome by wiping out or disrupting the natural composition of both good and bad bacteria. With a disrupted microbiome, resistant bacteria can take over (or colonize) and the body is less able to defend against infection, putting people at risk for potentially untreatable illnesses.
Microbiomes disrupted by antibiotics are vulnerable to infections by tough-to-kill germs such as Methicillin-resistant Staphylococcus aureus (MRSA), Carbapenem-resistant Enterobacteriaceae (CRE), Clostridium difficile (C. difficile), and E. coli. These patients can carry drug-resistant bacteria and can easily spread bacteria to other people, especially those who also have a disrupted microbiome.
Antibiotics are life-saving medicines, but they also change, unbalance, and disrupt your microbiome. This change could put people at risk for drug resistant infections.
CDC is conducting applied research on the microbiome to identify effective public health approaches that protect people, their microbiomes, and the effectiveness of antibiotics. CDC is investing in research and collaborating with investigators to determine:
- How Antibiotics Disrupt a Healthy Microbiome – CDC and investigators will study novel strategies that can protect and restore the microbiome, and determine how exposure to antibiotics early in life affects microbiome development.
- How a Disrupted Microbiome Puts People at Risk – CDC and investigators will develop a predictive index that identifies a patient’s risk of disruption from a specific antibiotic, to carry antibiotic-resistant bacteria, or become infected with one. CDC and investigators will also work to develop and test microbiome measurements that monitor a patient’s risk for disruption, and assess enhanced infection control triggers.
- How Antibiotic Stewardship Can Protect the Microbiome – CDC and investigators will improve strategies to tailor antibiotic stewardship to a patient’s individual microbiome, as well as assess how to fit antibiotic stewardship to a specific population of patients (e.g., hospital unit, nursing home, doctor’s office).
See a more extensive list of AR Solutions Initiative projects, including those related to the microbiome, below.
Innovations to Track & Prevent Antibiotic-Resistant Infections
To combat antibiotic resistance effectively, CDC is working to better understand antibiotic-resistant infections found across healthcare and the community—like drug-resistant healthcare-associated infections and foodborne infections. CDC and investigators will create innovative prevention and tracking strategies to protect people from these infections and stop spread.
See a more extensive list of AR Solutions Initiative research investigations, including innovative prevention and tracking across healthcare and the community, below.
Research Topics
Microbiome Assessment & Intervention
Innovations to Track & Prevent AR across Healthcare & the Community
AR Solutions Initiative: Microbiome Factsheet
Infographic Details
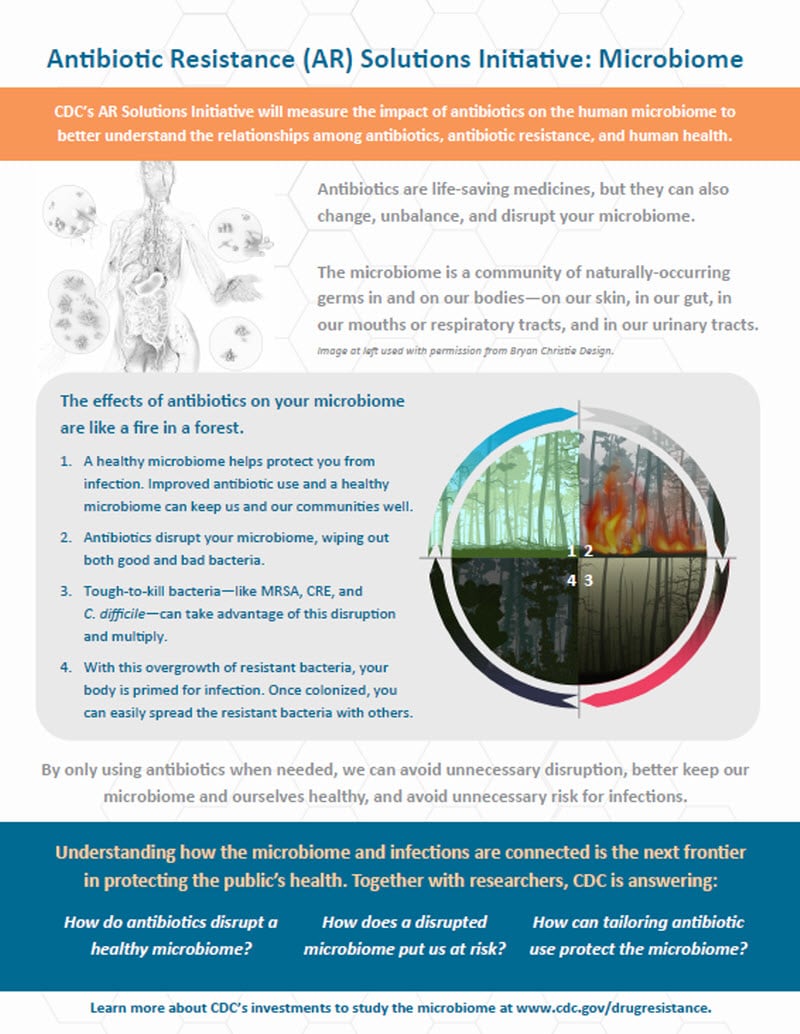
Antibiotic Resistance (AR) Solutions Initiative: Microbiome
CDC’s AR Solutions Initiative will measure the impact of antibiotics on the human microbiome to better understand the relationships among antibiotics, antibiotic resistance, and human health
Antibiotics are life-saving medicines, but they can also change, unbalance, and disrupt your microbiome.
The microbiome is a community of naturally-occurring germs in and on our bodies—on our skin, in our gut, in our mouths or respiratory tracts, and in our urinary tracts.
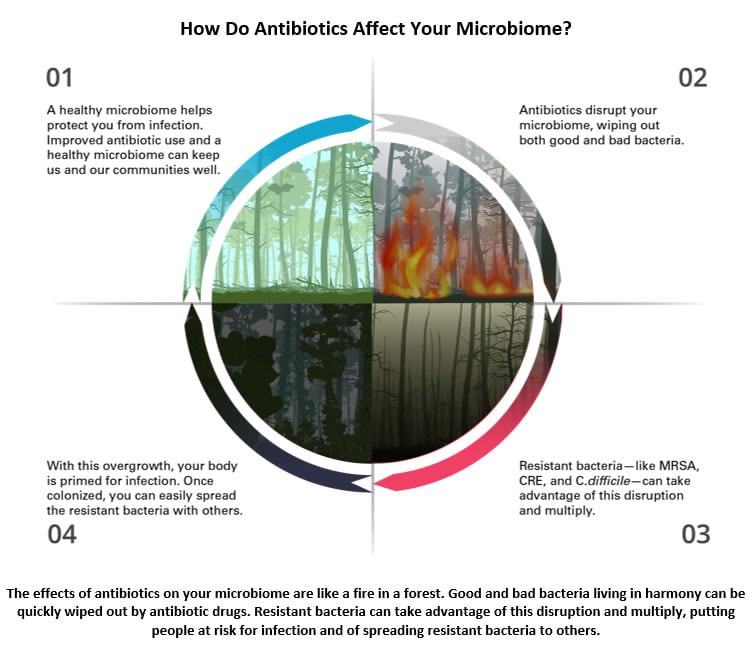
The effects of antibiotics on your microbiome are like a fire in a forest.
- A healthy microbiome helps protect you from infection. Improved antibiotic use and a healthy microbiome can keep us and our communities well.
- Antibiotics disrupt your microbiome, wiping out both good and bad bacteria.
- Tough-to-kill bacteria—like MRSA, CRE, and C. difficile—can take advantage of this disruption and multiply.
- With this overgrowth of resistant bacteria, your body is primed for infection. Once colonized, you can easily spread the resistant bacteria with others.
By only using antibiotics when needed, we can avoid unnecessary disruption, better keep our microbiome and ourselves healthy, and avoid unnecessary risk for infections.
Understanding how the microbiome and infections are connected is the next frontier in protecting the public’s health. Together with researchers, CDC is answering:
- How do antibiotics disrupt a healthy microbiome?
- How does a disrupted microbiome put us at risk?
- How can tailoring antibiotic use protect the microbiome?
Learn more about CDC’s investments to study the microbiome at www.cdc.gov/drugresistance.






















.jpg)










No hay comentarios:
Publicar un comentario