
COVID-19 could compromise key element of immune response
Researchers at the University of Melbourne, Monash University, James Cook University have made the unsettling discovery that infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) might compromise the activation of the CD8+ T-cell responses that would usually ameliorate disease and drive recovery in cases of respiratory disease.
Using a combination of peptide prediction and in vitro peptide stimulation, Katherine Kedzierska and the team found that while SARS-CoV-2 infection did stimulate CD4+ T-cell responses that were comparable to those seen with other viral infections, the CD8+ T cells that would usually target the virus were at low prevalence and less than optimal phenotype for viral elimination.
The SARS-CoV-2-specific response was ten times lower than would usually be found for CD8+ T-cells targeting the viral Epstein-Barr Virus (EBV) or influenza A (IAV), for example.
The team says further research is needed to provide a more detailed picture of CD8+ T-cell responses in coronavirus disease 2019 (COVID-19) since priming with an appropriate vaccine could be highly valuable in terms of optimizing protective CD8+ T-cell immunity.
A pre-print version of the paper is available on the server medRxiv*, while the article undergoes peer review.
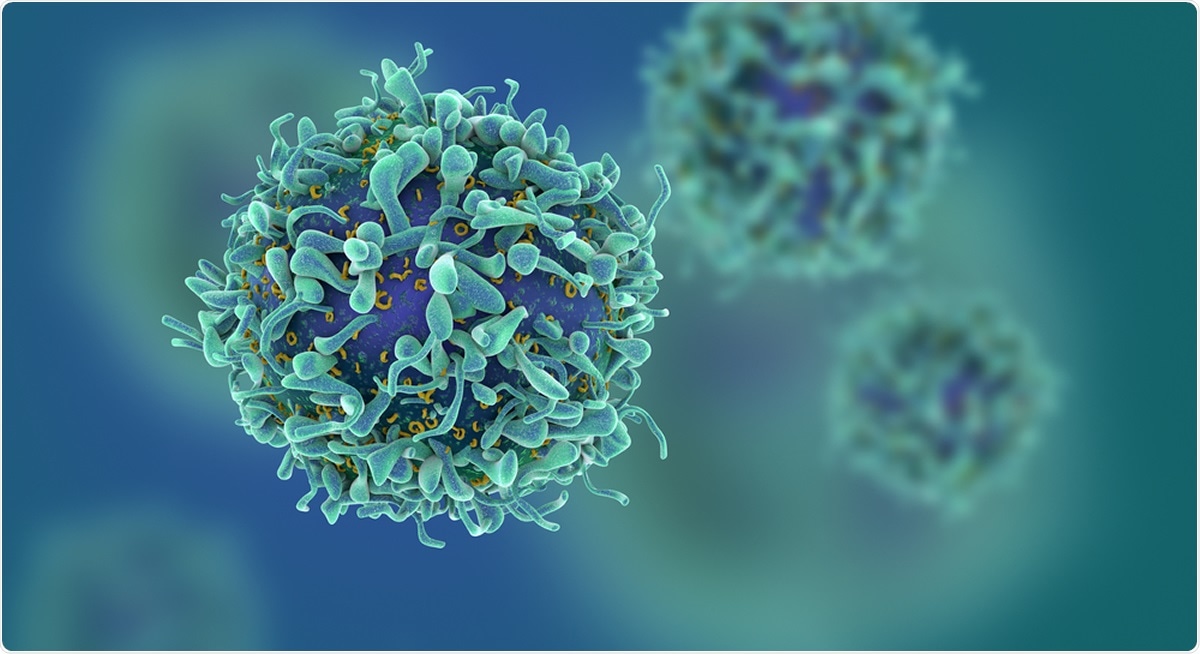
Study: Suboptimal SARS-CoV-2-specific CD8+ T-cell response associated with the prominent HLA-A*02:01 phenotype. Image Credit: Fusebulb / Shutterstock
Much remains unknown about the immune response to COVID-19
The current SARS-CoV-2 pandemic that continues to sweep the globe has now led to 22.53 million infections and caused more than 790,000 deaths.
Although the majority of infections only cause mild disease and are short-lived, around 12 to 18% of patients with COVID-19 develop severe disease and require hospitalization. Furthermore, of those who do develop mild disease or are even asymptomatic, the underlying pathology may still be present.
Much remains unknown about the immune response to COVID-19, and an improved understanding is urgently needed if any immunopathology is going to be managed appropriately and vaccine development optimized.
Virus-specific CD8+ T-cells are generally thought to play a role in clearing viral infection in the acute immune response to respiratory infection, where an established CD8+ T-cell memory response provides future protection against severe disease.
Survivors of the 2002-3 SARS-CoV-1 outbreak, for example, still maintain populations of CD4+ and CD8+ cells that are specific to the virus.
For SARS-CoV-2, evidence suggests that virus-specific T-cells are being produced. A previous study by Kedzierska and team found CD4+ T-follicular helper cells and activated CD38+ HLA-DR+ CD8+ T-cells in the blood of patients with COVID-19 three days before recovery, suggesting that these cells were involved in resolving disease.
However, another study showed that some of the SARS-CoV-2 specific CD8+ T cells in peripheral blood exhibited an “exhausted” phenotype, say the authors.
“Clearly, it is a matter of urgency to develop a better understanding of the integrity of the acute CD8+ T-cell response in COVID-19 and how this impacts on disease outcome,” they write.
What did the current study involve?
To investigate, the researchers applied peptide prediction and in vitro peptide stimulation using peptides from the SARS-CoV-2 Spike, Nucleocapsid, and Membrane proteins.
The team identified two novel HLA-A*02:01-restricted SARS-CoV-2 epitopes (A2/S269-277 and A2/Orf1ab3183-3191) in individuals with COVID-19.
Using a peptide-HLA enrichment technique, the researchers determined the frequency and activation profiles of the SARS-CoV-2-specific CD8+ T-cell response in individuals with acute COVID-19 infection, convalescent individuals, and uninfected donors.
Assessment of CD8+ T cell populations generated with the two novel epitopes showed that the more prominent A2/S269+ CD8+ T cell population was comparable to that seen in acute or convalescent patients positive for HLA-A*02:01.
However, although the CD8+ T cell population was higher than in uninfected HLA-A*02:01-positive donors, it was lower compared with the populations that are typically generated in response to EBV and IAV epitopes.
The CD8+ T-cells lacked activation markers
Further analysis of the A2/S269+ CD8+ T-cells from recovered patients revealed that A2/S269+ CD8+ T-cells generally lacked the important activation markers CD38, HLA-DR, PD-1, and CD71.
In summary, the authors say, that while the CD4+ T cell response was similar to that found in other viral infections, the virus-activated CD8+ T cells that target SARS-CoV-2 peptides presented by the HLA-A*02:01 glycoprotein were both low in number and of a phenotype that was suboptimal for viral clearance.
Further investigation is needed to identify CD8+ T cell epitopes across many HLA class I alleles and SARS-CoV-2 proteins and better determine the CD8+ T-cell responses and their activation profiles in COVID-19, advise Kedzierska and colleagues.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Kedzierska K, et al. Suboptimal SARS-CoV-2-specific CD8+ T-cell response associated with the prominent HLA-A*02:01 phenotype. medRxiv 2020. doi: https://doi.org/10.1101/2020.08.17.20176370

































No hay comentarios:
Publicar un comentario