
Fibromyalgia and Gut Health: SIBO and IBS
Skip to
- Fibromyalgia and irritable bowel syndrome
- What are the common clinical features between IBS and fibromyalgia?
- Does fibromyalgia and IBS have common etiologies?
- Fibromyalgia and small intestinal bacterial overgrowth (SIBO)
Fibromyalgia is characterized by chronic and widespread musculoskeletal pain and stiffness. Other common symptoms are extreme fatigue, sleep disturbance, memory and cognitive problems, and emotional distress.
The pain experienced in fibromyalgia is not caused by injuries or damages to the body tissues; instead, the pain basically results from altered pain signaling in the central and peripheral nervous systems that causes increased sensitivity to pain (pain amplification).
Fibromyalgia patients often have gastrointestinal problems, such as abdominal pain, bloating, and constipation, which are very similar to those observed in irritable bowel syndrome (IBS). Moreover, given the association between IBS and small intestinal bacterial overgrowth (SIBO), it has been hypothesized scientifically that fibromyalgia is associated with SIBO as well.
Fibromyalgia and irritable bowel syndrome (IBS)
IBS is a gastrointestinal (GI) tract disorder characterized by chronic abdominal pain, bloating, constipation, and diarrhea. Around 2/3 of IBS patients present with rheumatologic symptoms, such as muscle pain, headache, and skin rash.
Studies have found that IBS frequently coexists with fibromyalgia. The prevalence of fibromyalgia among IBS patients is almost 60%, and around 70% of fibromyalgia patients demonstrate IBS-like symptoms.
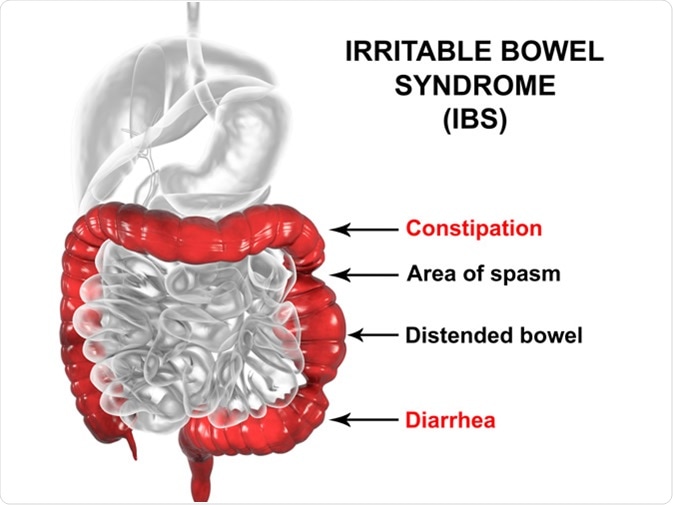
Irritable bowel syndrome IBS, 3D illustration showing spasms and distortion of large intestine. Image Credit: Kateryna Kon / Shutterstock
What are the common clinical features between IBS and fibromyalgia?
Although pain experienced in IBS (GI pain) and fibromyalgia (musculoskeletal pain) is different in nature and origin, both the conditions share some common clinical features.
Both IBS and fibromyalgia are more common in women. Studies have found that IBS is diagnosed in 14-24% of women and 5-19% of men; similarly, fibromyalgia is detected in 3.4% of women and 0.5% of men.
Although diagnosed as separate entities, both IBS and fibromyalgia are categorized as functional pain disorders without obvious structural or biochemical etiologies.
In most of the cases of IBS and fibromyalgia, stressful life events or chronic stressful condition is associated with the disease development or augmentation of symptom severity.
Patients suffering from IBS or fibromyalgia present with some common symptoms, including sleep disturbance, fatigue, and emotional distress. These patients are often benefited from psychological and behavioral therapies.
Does fibromyalgia and IBS have common etiologies?
IBM pathogenesis primarily involves visceral hypersensitivity, altered gut wall compliance and intestinal motility, and emotional distress.Fibromyalgia is primarily associated with somatic (muscles and joints) hypersensitivity, stiffness, fatigue, and sleep disturbance.
Studies involving patients with only IBS or both IBS and fibromyalgia have indicated that IBS patients have reduced somatic pain sensation, whereas patients suffering from both IBS and fibromyalgia have increased somatic pain sensation (somatic hypersensitivity) similar to those with fibromyalgia. These findings suggest that a simultaneous presence of fibromyalgia makes IBS patients more sensitive to musculoskeletal pain.
Regarding processing of somatic and visceral pain information in the brain, it has been found that patients with both IBS and fibromyalgia share some common features:
- They have higher neural activity in the brain areas responsible for pain sensation
- Retrieval of the memory related to past pain experiences is higher in these patients
- They have increased level of attention or awareness in response to a stimulus
In other words, it can be said that brain processing of visceral and somatic pain sensation in patients with both IBS and fibromyalgia is uniquely different from that in patients with IBS or fibromyalgia alone. This suggests that both the conditions may have common etiology.
Fibromyalgia and small intestinal bacterial overgrowth (SIBO)
SIBO is a GI condition wherein normal aerobic and anaerobic bacteria of the colon overgrow into the small intestine, resulting in disruption of normal intestinal bacterial patterns. The condition is frequently diagnosed by lactulose breath test (LBT).
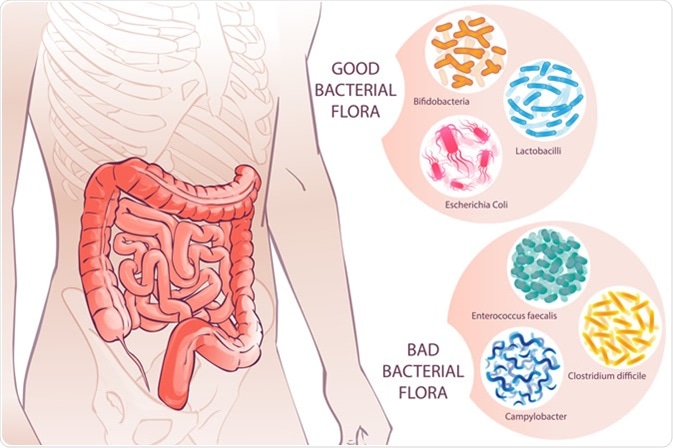
Bacterial Flora. Image Credit: first vector trend / Shutterstock
Studies have found that patients with IBS show abnormal results on LBT, and IBS patients have better clinical outcome after the normalization of LBT results with antibiotic treatments. Moreover, studies have shown that fibromyalgia patients show abnormalities on LBT, suggesting that both IBS and fibromyalgia are related to SIBO. However, the degree of abnormalities on LBT is generally higher in fibromyalgia patients than that in IBS patients.
Studies focusing on gut bacteria and pain sensation have demonstrated that bacterial endotoxins and endotoxin-related cytokines can increase sensitivity to pain. Additionally, the level of hydrogen produced by bacterial overgrowth (LBT) correlates with the degree of pain in fibromyalgia patients.
Lipopolysaccharide (LPS), a major component of gram-negative bacterial outer membranes, is found predominantly in the GI tract, and SIBO increases systemic absorption of LPS through the gut wall. Studies have shown that LPS triggers microglial activation, disruption of muscle mitochondria, peripheral pain sensitivity, and central sensitization. These findings indicate a possible connection between SIBO and symptom severity in fibromyalgia patients.
Studies have also shown that eradication of SIBO with antibiotics significantly improves the clinical outcome of fibromyalgia patients. Given the prevalence of GI co-morbidities in fibromyalgia patients, physicians should be aware of possible co-morbid GI symptoms while diagnosing or treating fibromyalgia patients.
Sources
- Chang L. The Association of Irritable Bowel Syndrome and Fibromyalgia. https://www.med.unc.edu/ibs/files/2017/10/Fibromyalgia-and-IBS.pdf
- Badgut.org. Fibromyalgia and irritable bowel syndrome. 2018. badgut.org/.../
- Yang T Y., et al. (2017). Risk for Irritable Bowel Syndrome in Fibromyalgia Patients. Medicine (Baltimore). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5411228/
- Pimentel M., et al. (2004). A link between irritable bowel syndrome and fibromyalgia may be related to findings on lactulose breath testing. Annals of the Rheumatic Diseases. https://ard.bmj.com/content/63/4/450#ref-1
- Kim Y S., et al. (2011). Why Should Gastroenterologists Know About Fibromyalgia? Common Pathogenesis and Clinical Implications. J Neurogastroenterol Motil. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042210/
- Vasquez A. (2016). Neuroinflammation in fibromyalgia and CRPS is multifactorial. Nature Reviews Rheumatology. https://www.nature.com/articles/nrrheum.2016.25
Further Reading
Last Updated: Jun 10, 2019

































No hay comentarios:
Publicar un comentario