
Studies Identify Therapies That May Delay Melanoma Recurrence after Surgery
October 19, 2017, by NCI Staff
Two recent clinical trials have identified treatments that may delay cancer from returning in some patients with melanoma. Patients in both trials had advanced melanoma that was surgically removed, and each trial tested different forms of post-surgical, or adjuvant, therapy.
One trial tested an immunotherapy drug known as an immune checkpoint inhibitor. The other tested the combination of two targeted therapies in patients whose tumors had a specific genetic mutation.
Both studies were reported at the European Society for Medical Oncology annual conference and published September 10 in the New England Journal of Medicine.
“Patients with stage III melanoma currently have limited options for adjuvant therapy and the current FDA-approved therapies have not been widely used because they can cause significant side effects,” said William Sharfman, M.D., of the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, who was an investigator on the targeted therapy trial.
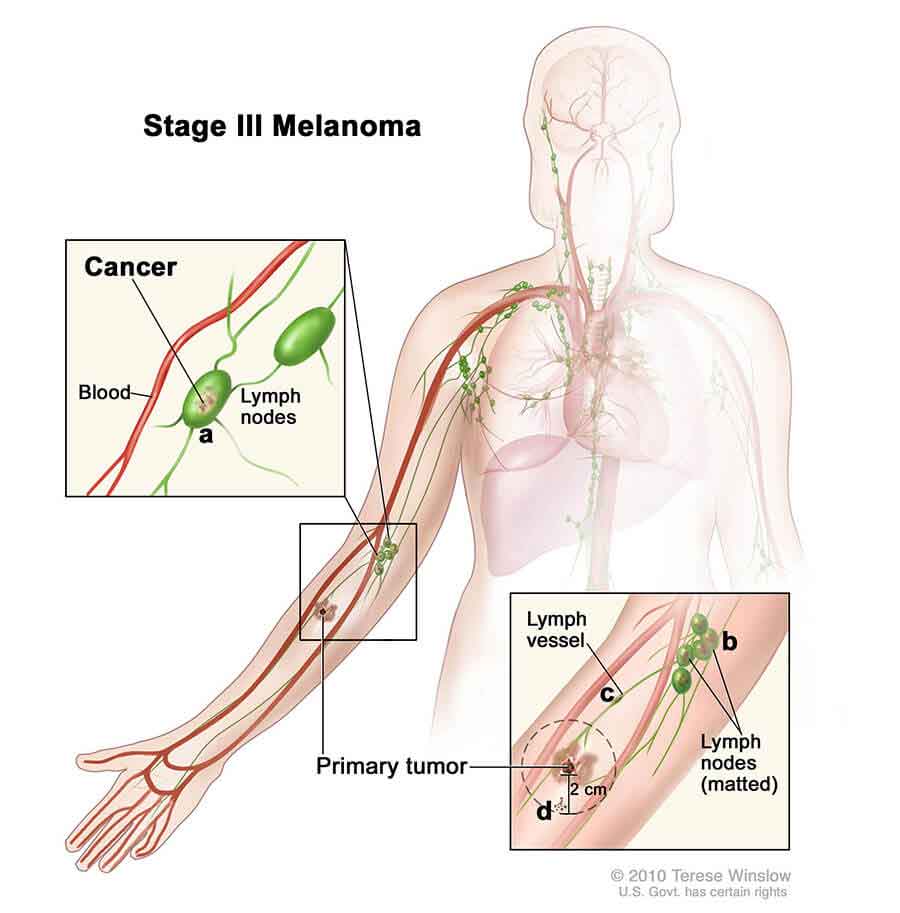
Stage III melanoma is skin cancer that has spread to one or more lymph nodes, but has not spread to other organs.
If the treatments tested in the trials are approved by the Food and Drug Administration (FDA) as adjuvant therapies for patients with melanoma, Dr. Sharfman said, “we would probably see most patients with stage III melanoma getting adjuvant therapy. So these trials are game changing.”
Immune Checkpoint Inhibitors as Adjuvant Therapy
Cancer cells can activate so-called “checkpoint proteins” on immune cells to thwart an immune response against the tumor. Immune checkpoint inhibitors, such as nivolumab (Opdivo®) and ipilimumab (Yervoy®), block the actions of these proteins and allow an immune response against the tumor to occur.
In 2015, FDA approved ipilimumab as an adjuvant therapy for patients with stage III melanoma that has been removed by surgery. Ipilimumab is also approved in combination with nivolumab to treat some patients with unresectable or metastatic melanoma.
The investigators conducting the CheckMate 238 trial randomly assigned 906 patientswith surgically-removed stage III or IV melanoma to receive adjuvant treatment with nivolumab or ipilimumab for 1 year.
The study was sponsored by Bristol-Myers Squibb, the manufacturer of both nivolumab and ipilimumab.
The trial’s primary endpoint was recurrence-free survival—the length of time from randomization to when the patient’s cancer returned at the same site, or spread to nearby lymph nodes or distant organs.
After 18 months, 66% of patients in the nivolumab group and 53% in the ipilimumab group did not have cancer recurrence. Compared with ipilimumab, nivolumab increased the 12-month recurrence-free survival rate for patients with stage III and stage IV melanoma.
Currently, there is no FDA-approved adjuvant therapy for patients with surgically-removed stage IV melanoma, so there is a significant need for an effective therapy for these patients, noted Dr. Sharfman.
Nivolumab treatment also led to longer metastasis-free survival (the length of time between randomization and cancer metastasis) than ipilimumab, they found.
More patients who received ipilimumab than who received nivolumab reported serious treatment-related side effects (46% versus 14%). Side effects led 43% of ipilimumab-treated patients to discontinue treatment, compared with 10% of nivolumab-treated patients.
Patients in the trial haven’t yet been followed long enough for the investigators to determine whether nivolumab improved overall survival compared with ipilimumab.
Overall survival is considered a more important endpoint, and an increase in recurrence-free survival does not necessarily translate into an improvement in overall survival, said Elad Sharon, M.D., of NCI’s Cancer Therapy Evaluation Program, who was not involved in either trial. That’s because many patients who start with ipilimumab after surgery may later get access to nivolumab or a similar drug if their cancer returns, Dr. Sharon said.
Some clinicians and patients opt against adjuvant therapy with ipilimumab because of the harsh side effects. The finding that nivolumab caused fewer side effects than ipilimumab may make it oncologists’ preferred choice for adjuvant therapy—even if overall survival turns out to be similar for the two drugs—Dr. Sharon said.
Targeted Therapy as Adjuvant Therapy
About 50% of people with melanoma have mutations in the BRAF gene that lead to constant activation of a signaling pathway that fuels tumor growth. The targeted therapies dabrafenib (Tafinlar®) and trametinib (Mekinist®), which block the action of proteins that are part of this pathway, are approved by FDA as a combination therapy to treat patients with metastatic or unresectable melanoma that has one of two specific BRAF mutations.
In the COMBI-AD trial, 870 patients with surgically removed stage III melanoma with either of these BRAF mutations were randomly assigned to treatment with the combination of dabrafenib plus trametinib or with placebo for 1 year. The study was sponsored by GlaxoSmithKline and Novartis.
Recurrence-free survival, the trial’s primary endpoint, was longer for patients in the combination therapy group than patients in the placebo group, the investigators found. The estimated 3-year recurrence-free survival rate was 58% for the combination therapy group and 39% for the placebo group.
Fewer patients in the combination therapy group than in the placebo group died from cancer. The combination therapy led to an increase in overall survival compared with placebo, the investigators found.
Because patients who had cancer recurrence were allowed to try other therapies, “it’s hard to interpret what the difference in overall survival means,” noted Dr. Sharfman. Among participants in the combination therapy and placebo groups, 34% and 50%, respectively, received another treatment (including surgery, radiation, targeted therapy, immunotherapy, or chemotherapy) after their cancer recurred.
More patients in the combination therapy group than the placebo group reported a serious side effect leading to treatment discontinuation, dose reductions, and treatment interruptions. The side effect profile for dabrafenib and trametinib was similar to what has been observed in separate trials, and in general patients tolerated the drug combination well, the investigators noted.
Considerations for Adjuvant Therapies
All patients in both trials who had stage III disease had a complete lymph node dissection—meaning that lymph nodes in the area around the tumor had been surgically removed. But a recent clinical trial demonstrated that, for patients with melanoma, complete lymph node dissection did not improve survival when compared with watchful observation of cancer growth.
“The question is, can patients go on to adjuvant therapy without complete node dissection?” said Dr. Sharfman. “We don’t currently know if immunotherapy or targeted therapy works better for patients who have had a node dissection” compared to those who haven’t, he explained.
Dr. Sharfman expects that nivolumab and the dabrafenib-trametinib combination will be approved by FDA as an adjuvant therapy for these patients. At that point, Dr. Sharfman said, an important question will be, “how to choose one of these regimens over the other?”
For some patients, the absence of a BRAF mutation or tumor stage could facilitate that decision, he explained. But for those with a mutation, a clinical trial directly comparing the two treatments would be the only way to definitively answer the question.





















.png)










No hay comentarios:
Publicar un comentario