
What is CRISPR gene editing, and how does it work?
by Merlin Crossley | 3 Feb 2018 | 1 comment

You’ve probably read stories about new research using the gene editing technique CRISPR, also called CRISPR/Cas9. The scientific world is captivated by this revolutionary technology, since it is easier, cheaper and more efficient than previous strategies for modifying DNA.
The term CRISPR/Cas9 stands for Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR associated protein 9. The names reflect important features identified during its discovery, but don’t tell us much about how it works, as they were coined before anyone understood what it was.
What does CRISPR/Cas9 do?
CRISPR/Cas9 is a system found in bacteria and involved in immune defence. Bacteria use CRISPR/Cas9 to cut up the DNA of invading bacterial viruses that might otherwise kill them.
Today we’ve adapted this molecular machinery for an entirely different purpose – to change any chosen letter(s) in an organism’s DNA code.
We might want to correct a disease-causing error that was inherited or crept into our DNA when it replicated. Or, in some cases, we may want to enhance the genetic code of crops, livestock or perhaps even people.
So do we just snip the unwanted gene out and replace it with a good one?
We first have to remember that animals and plants are composed of millions of cells, and each cell contains the same DNA. There is no point editing just one cell: we would have to edit the same gene in every single cell. We’d have to snip out millions of genes and paste in millions of new ones.
And not all cells are easy to get to – how could we reach cells buried in our bones or deep within a brain?
A better approach is to start at the beginning and edit the genome while there is only one cell – a very early embryo.
So, all we need is a giant microscope and a tiny pair of scissors. And that is basically what we use.
Cas9 is the technical name for the virus-destroying “scissors” that evolved in bacteria. The CRISPR part of the name comes from repeat DNA sequences that were part of a complex system telling the scissors which part of the DNA to cut.
Find, cut and then paste
In order to target our Cas9 scissors, we link them to an artificial guide that directs them to the matching segment of DNA.
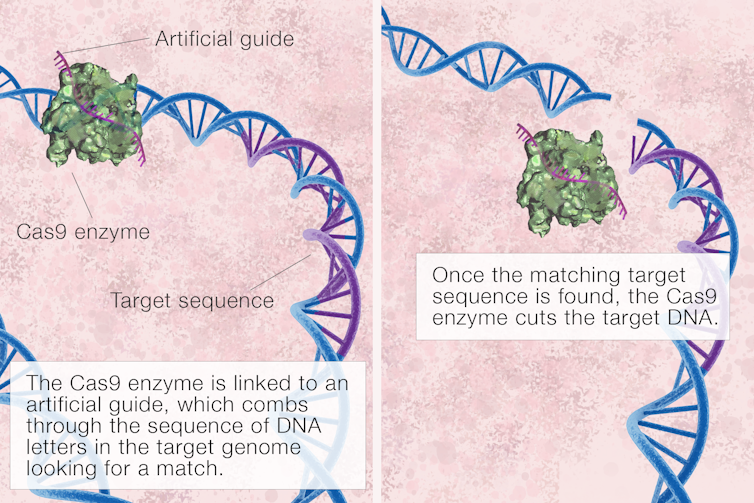
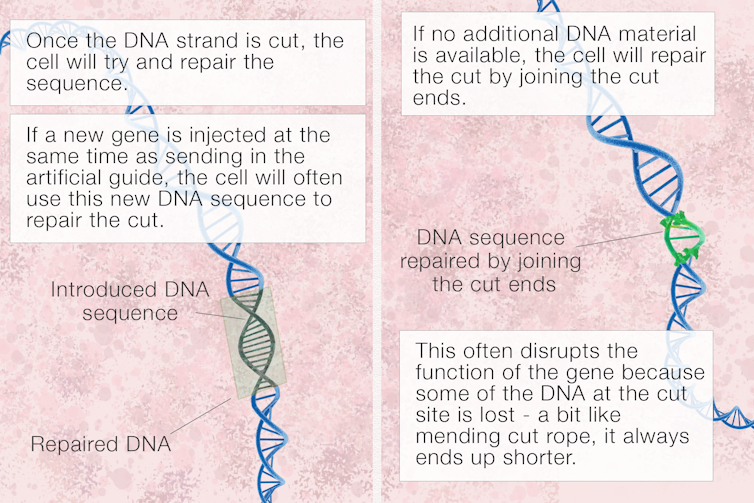
Once the Cas9 scissors cut the DNA just where we intend, the cell will try to repair the break using any available DNA it can find. So, we also inject the new gene we want to insert.
But how does the new gene find the right place to embed itself? Imagine you wanted to put in the last piece of a jigsaw puzzle with 3 billion pieces, and it’s inside a cell, filled with goop like a passionfruit.
What you’d do is fabricate a jigsaw piece of precisely the right shape and inject it into the passionfruit. Then it’s just a case of jiggling around until eventually the piece finds its way to the correct part of the puzzle and slots into the only place it fits.
You don’t need to be able to see the DNA in our genome through the microscope – it’s too small. And you don’t really have to jiggle either – random diffusion (called Brownian motion) will always deliver the jigsaw piece to the place where it fits in the end.
First, the guide will jiggle along and find the right place for the scissors to cut, and then the new donor DNA will similarly line up where it fits and will be permanently stitched into the DNA strand via natural DNA repair mechanisms.
Recently, though, new CRISPR editing systems have been created that don’t even require a cut through the DNA. In this case, the CRIPSR/Cas and guide system can deliver an enzyme to a particular gene and alter it, changing perhaps an A to a G or a C to a T, rather than cutting anything out or putting anything in.
What are we doing with CRISPR/Cas9?
Most experiments use mouse embryos or cells grown in petri dishes in artificial liquid designed to be like blood. Other researchers are modifying stem cells that may then be re-injected into patients to repopulate damaged organs.
Only a few labs around the world are actually working with early human embryos. This research is highly regulated and carefully watched. Others work on plant cells, as whole plants can be grown from a few cells.
As we learn more, the scope of what we can do with CRISPR/Cas9 will improve. We can do a lot, but every organism and every cell is different. What’s more, everything in the body is connected, so we must think about unexpected side effects and consider the ethics of changing genes. Most of all we, as a society, should discuss and agree what we wish to achieve.
Merlin Crossley, Deputy Vice-Chancellor Academic and Professor of Molecular Biology, UNSW. This article was originally published on The Conversation. Read the original article.

For years bioethicists of a utilitarian cast have argued that conscientious objection has no place in medicine. Now Canadian courts are beginning to put their stamp of approval on the extinction of doctors’ right to refuse to kill their patients.
The Superior Court of Justice Division Court of Ontario ruled this week that if doctors are unwilling to perform legal actions, they should find another job (see report in BioEdge).
The case is sure to be appealed, but if the doctors championing conscientious objection fail, the consequences will be dire. Throughout Canada, doctors would be required to refer for euthanasia. If they refuse, they will be hounded out of their profession, or, at best, shunted into specialties where the question will not arise, like pathology or dermatology.
This ruling shows how quickly tolerance vanishes after euthanasia has been legalised. In the Carter decision which legalised it, Canada’s Supreme Court explicitly stated that legalizing euthanasia did not entail a duty on the part of physicians to provide it. Now, however, 18 months and more than a thousand death after legalisation, conscientious objection is at risk.
It also shows how vulnerable religious-based arguments can be. The plaintiffs contended that referring patients violated their right to religious freedom. While this is true, is this the main ground for conscientious objection? As several doctors pointed out in the Canadian Medical Association Journal last year, “Insofar as all refusals of therapy are ultimately justified by the ethical belief that the goal of therapy is to provide benefit and avoid harm, all treatment refusals are matters of conscience.”
The Superior Court of Justice Division Court of Ontario ruled this week that if doctors are unwilling to perform legal actions, they should find another job (see report in BioEdge).
The case is sure to be appealed, but if the doctors championing conscientious objection fail, the consequences will be dire. Throughout Canada, doctors would be required to refer for euthanasia. If they refuse, they will be hounded out of their profession, or, at best, shunted into specialties where the question will not arise, like pathology or dermatology.
This ruling shows how quickly tolerance vanishes after euthanasia has been legalised. In the Carter decision which legalised it, Canada’s Supreme Court explicitly stated that legalizing euthanasia did not entail a duty on the part of physicians to provide it. Now, however, 18 months and more than a thousand death after legalisation, conscientious objection is at risk.
It also shows how vulnerable religious-based arguments can be. The plaintiffs contended that referring patients violated their right to religious freedom. While this is true, is this the main ground for conscientious objection? As several doctors pointed out in the Canadian Medical Association Journal last year, “Insofar as all refusals of therapy are ultimately justified by the ethical belief that the goal of therapy is to provide benefit and avoid harm, all treatment refusals are matters of conscience.”
 Michael Cook Editor BioEdge |
NEWS THIS WEEK
by Michael Cook | Feb 03, 2018
But are the protests ill-informed?by Michael Cook | Feb 03, 2018
High dosage led to toxicity and animal deathsby Xavier Symons | Feb 03, 2018
An Ontario court has told a group of doctors that they must refer for MAiD.by Xavier Symons | Feb 03, 2018
A court has ordered life support to be withdrawn from an 11-month-old boy.by Xavier Symons | Feb 03, 2018
Are British doctors obliged to withdraw life support if requested by a patient?by Xavier Symons | Feb 03, 2018
Should cancer sufferers have greater access to experimental treatment?IN DEPTH THIS WEEK
by Merlin Crossley | Feb 03, 2018
It's an exciting field, with much to discoverBioEdge
Phone: +61 2 8005 8605
Mobile: 0422-691-615





















.png)










No hay comentarios:
Publicar un comentario